Disponible seulement en version anglaise. Cette étude de cas est disponible en français. Este estudio de caso está disponible en español.
Introduction
This report, conducted by the National Collaborating Centre for Infectious Diseases (NCCID) in partnership with the Winnipeg Regional Health Authority Integrated Tuberculosis Services (WRHA-ITBS) and BridgeCare Clinic, presents an in-depth review and analysis of the model of latent tuberculosis infection (LTBI) management and promising treatment completion outcomes at BridgeCare Clinic in Winnipeg, Canada. NCCID is one of six National Collaborating Centres (NCCs) funded by the Public Health Agency of Canada to facilitate the use of evidence and emerging research in Canadian public health practice, programs and policy. As part of its commitment to eliminating tuberculosis in Canada, NCCID has partnered with the WRHA and other health bodies across Canada to share and exchange knowledge on innovative and promising approaches in tuberculosis (TB) prevention and care. In this report we review the BridgeCare Clinic model of integrated TB services for government-assisted refugees as an approach to improve LTBI management outcomes in priority populations. Activities involved in this report included: a review of literature on TB treatment completion outcomes amongst comparable models and systems of TB care; several in-depth consultations and interviews with clinic and TB program staff; and an analysis of TB program data at BridgeCare Clinic. In the first part of this report, we describe the organization of TB services in Manitoba and present an overview of TB epidemiology, highlighting the importance of LTBI treatment among foreign born populations. This is followed by a description of activities and methods and a presentation of results from our literature search, in-person interviews and data analysis. At the end, we discuss the findings and present some considerations for continued TB management among refugees in Winnipeg.
TB Care in Manitoba
In Manitoba, TB management is distributed amongst the five Regional Health Authorities (RHA) in Manitoba (1). The WRHA, as a Regional Health Authority, is responsible for providing health care to people living in the city of Winnipeg, and the surrounding rural municipalities of East and West St. Paul and the town of Churchill in northern Manitoba. The WRHA also provides health care support and specialty referral services to Manitobans who live outside of the areas described above, as well as residents of northwestern Ontario and Nunavut who require the services and expertise available within the Region (2). Until 2006, TB services in Manitoba were delivered within a centralized system; responsibility for the TB program rested at the provincial level, with only a single provider for TB care in the province. However, in 2006 a gradual decentralization of services began, with the transference of responsibility for the TB program to RHAs and the provision of TB services in more than one facility. Currently, ITBS is the organizational structure which facilitates and delivers quality TB screening and care to people throughout Winnipeg and provides consultative support to other RHA’s in Manitoba (3). At present, Non-Complex LTBI assessment and management is provided at three primary care sites in Winnipeg, under two different service models. These include the Primary Care Specialty model at Klinic and Access Downtown, and the BridgeCare Clinic model, which offers comprehensive health care to newly arrived, government-assisted refugees (4). BridgeCare Clinic opened in November 2010 and has offered LTBI screening and treatment since 2014 under the decentralized intersectoral model for TB services recently established by the WRHA. Preliminary findings from Manitoba Health, Seniors and Active Living on this new model of urban TB care have been encouraging (5), providing the impetus to conduct a more in-depth analysis. In particular, a new pre-release report described positive outcomes in a population based analysis on LTBI treatment completion outcomes in Winnipeg from 2012 to 2014. Investigators used the provincial Drug Program Information Network (DPIN) database to describe the demographic and geographical distribution of individuals receiving LTBI treatment, as well as evaluate LTBI treatment completion rates in Winnipeg. The results indicated that, “Key LTBI primary care sites” (Klinic, Access Downtown and BridgeCare Clinic), were at least as successful as chest specialists at achieving good treatment outcomes (>75% completion rates) (5). However, as these findings were based on aggregated data across clinics and proxy measures for treatment completion (prescription dispensing records), further research to explore heterogeneity in outcomes is warranted. In this report, we compared the findings from Manitoba Health, Seniors and Active Living to those found by others studying treatment completion outcomes within comparable models and systems of TB care. As well, we examined treatment completion outcomes at BridgeCare Clinic using clinic and program-level data from January 2015 to October 2016.
1.0 Epidemiology of Tuberculosis in Canada and Manitoba
1.1. Canada
Canada has one of the lowest TB rates in the world (6) and rates of new TB cases have been declining overall. However, there are significant disparities in certain population groups and geographic regions, as foreign born and Indigenous men and women are disproportionately affected by TB. Among the foreign born, the proportion of TB cases has increased during the past 40 years. Eleven percent of the reported cases of TB among foreign born women and men between 2000 and 2010 were reported within the first year of arrival, 22% within the second year, and 44% within five years. The proportion of TB cases reported among foreign born people from the Western Pacific and South-East Asia (World Health Organization (WHO) epidemiologic regions) increased during the period 1970 to 2010. The TB incidence rate among males has been historically higher than among females, but the differential has decreased over time (7).
According to the 2016 Canadian TB pre-release report, in 2014, there were 1,568 cases of active TB reported, 5% less than in 2013. Active TB incidence for 2014 was 4.7 per 100,000 population with new cases accounting for 94% of the active TB cases reported. There is geographic heterogeneity in TB incidence rates in Canada with the highest rates in Nunavut, Yukon, Manitoba and the Northwest Territories. Between 2004 and 2014 TB incidence rates were stable across age groups (8).
In 2014, TB cases among the foreign born population accounted for 69% of reported cases (incidence rate of 20.4 per 100,000 population) in Canada, despite the number of foreign born residents only representing 22% of the total population of Canada. Those persons from the Western Pacific Region had the highest percentage of reported foreign born cases (44%), and of these cases 78% were from China and the Philippines. However, the highest incidence rate (40.5 per 100,000 population) occurred among men and women born in regions of Africa with high HIV prevalence (8). (See Annex 1 for a list of high TB burden countries according to WHO (9).)
Similarly, Indigenous populations are significantly over represented in new cases of TB. In 2014, the incidence rate among Métis people was 3.2 per 100,000 population, followed by a rate of 19.3 per 100,000 population among First Nations people, and the highest rates were seen among the Inuit people, at 198.3 per 100,000 population (8).
1.2. Manitoba
For more than 30 years the TB incidence rate in Manitoba has been consistently higher than the TB incidence rate in Canada (1). During 2014, Manitoba reported 135 cases of active TB for an incidence rate of 10.5 cases per 100,000 population, more than twice the Canadian TB incidence rate. Adults aged 35 to 44 years represented the highest number of cases with an incidence rate of 18.4 per 100,000 population (8).
Contrary to national data, the foreign born population accounted for only 32.6% of cases in Manitoba (incidence rate 20.5 per 100,000 population). The most frequent origin of foreign born cases was the Western Pacific Region with 26 out of 44 cases (59%) similar to national trends. Indigenous persons accounted for 62.2% of the cases in Manitoba (incidence rate 37.7 per 100,000 population). Among the Indigenous persons with TB, 83 out of 84 cases identified as First Nations (8).
2.0 Activities and Methods
The information gathered for this report involved: i) a literature review focused on TB treatment completion outcomes among primary care and other decentralized models for TB care; ii) an orientation to BridgeCare Clinic and interviews with its staff to better understand the LTBI program and explore facilitators and barriers to LTBI screening and treatment; and iii) an analysis of BridgeCare Clinic TB program data to help validate the findings from the Manitoba Health, Seniors and Active Living pre-release report on LTBI treatment completion outcomes in primary care settings (5).
2.1. Literature Review Method
The literature review was conducted using a PUBMED electronic database. The following search terms were included: “(tuberculosis OR latent tuberculosis) AND (care model OR ambulatory care OR patient-centered care OR patient care team OR physicians, primary care OR family health OR quality assurance, health care OR decentralization OR holistic health OR integrated services OR focal point) AND (treatment outcome OR treatment completion)”. The search was limited to studies published before August 31st, 2016, in peer-reviewed journals in English, Spanish, and French. Over 500 study titles and abstracts were screened based on pre-defined inclusion and exclusion criteria.
Inclusion criteria:
- Quantitative and qualitative studies
- Peer-reviewed articles
- English, Spanish or French language
- Studies describing a model for TB care involving primary or family care, decentralized services, or integrated services
Exclusion criteria:
- Lack of TB treatment completion outcome measures
2.2. Information Gathering and Analysis at BridgeCare Clinic
Orientation and Interviews
A two hour BridgeCare Clinic orientation served to develop an understanding of the organization of the clinic, the care services provided and the staffing composition. One hour interviews with four BridgeCare Clinic staff were conducted to explore the facilitators and barriers to LTBI screening and treatment at the clinic, and to map the typical care pathway of a client screened for LTBI. These interviews were followed by consultations with two ITBS program members to further contextualize the findings.
During the interviews, five main questions were posed:
- How would you describe the process for LTBI screening and treatment for people that access BridgeCare Clinic?
- From your perspective, what do you think about the performance of LTBI screening and treatment processes at BridgeCare Clinic?
- What aspects of the LTBI screening and treatment process do you think contribute to positive outcomes?
- What aspects of the LTBI screening and treatment process do you think could be improved?
- At BridgeCare Clinic, what challenges do you encounter when conducting LTBI screening and treatment?
The orientation and interviews were performed on site at BridgeCare Clinic. Additionally, documents related to the LTBI program were collected and reviewed. These documents included TB guidelines and protocols used at the clinic, TB forms, details on the type of information collected in patient records/databases, and educational materials and resources for the public.
Program Data Review
The BridgeCare Clinic staff provided access to de-identified TB program data from January 2015 to October 2016, including basic demographic information (age, sex, country of birth), numbers of clients screened with Interferon Gamma Release Assay (IGRA), and the number of clients who were a) eligible for LTBI treatment, b) currently on LTBI treatment and c) completed treatment.
Global IGRA test result proportions were calculated, as well as proportions according to sex, country of birth, and mean age. Country of birth was categorized in one of six WHO regions (see Annex 2).
With 95% confidence, mean age between groups of negative and positive IGRA test results were compared with Student’s t-test. Chi-Squared tests were used to compare sex and country of birth proportions according to IGRA test results.
Only IGRA test positive results from 2015 were included in the analysis of LTBI treatment completion outcomes. Mean age was calculated as well as proportions for sex and country of birth categorized by WHO regions. A Chi-Squared test was used to compare the proportion of individuals with IGRA positive results that started LTBI treatment by sex.
3.0 Results
3.1. Literature Review
Over 500 titles were generated in the search. A subset of these articles was selected for abstract review and a smaller subset for full review. A description of the article selection process is provided in the flow chart below (Figure 1).
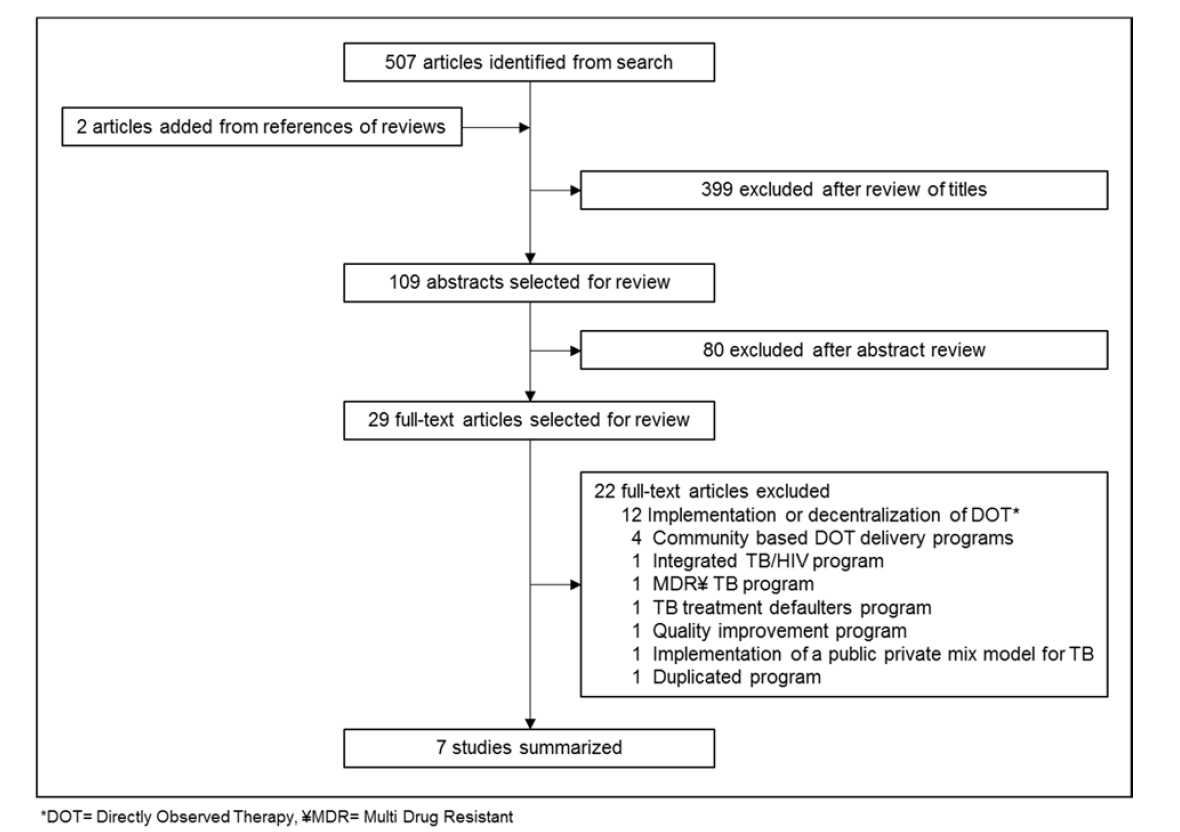
Figure 1. Inclusion and exclusion of studies retrieved from literature search.
Based on the titles, 399 papers were excluded and 109 papers were reviewed by abstracts. Of these, 29 full-text papers were reviewed. Seven of 29 papers reviewed were chosen for summary; they focused on decentralized and integrated care models for TB that were based on family or primary care. Of the seven papers, two were based in Canada, three in the United States, one in Brazil, and one in Taiwan. A brief description of the summarized studies is presented in Table 1. The first four papers we reviewed examined LTBI care; two focused on refugee populations. The last three papers presented an analysis of active TB care.
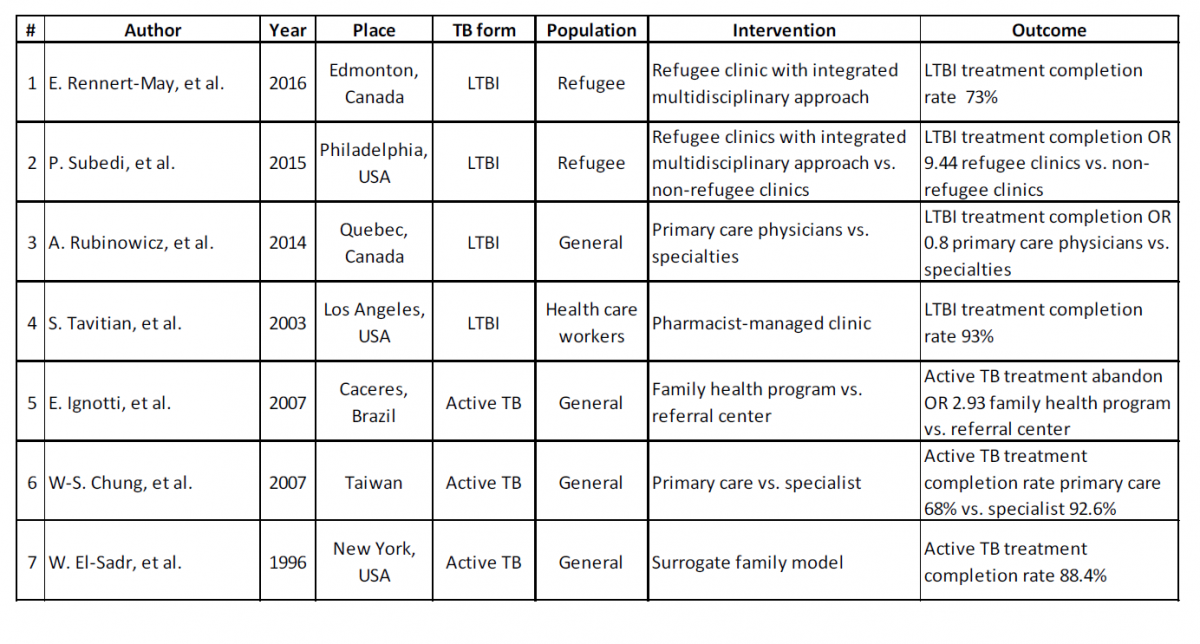
Table 1. Summary of seven studies included in the literature review.
Study 1, a 2016 study from Rennert-May et al. (10) describes a new screening program in Edmonton for government-assisted refugees after arrival. The program included evaluation within two weeks of arrival, integration of TB services with a general refugee health clinic, and the placement of a TST in most refugees, when indicated. Of 746 patients who successfully received a TST with reading, 265 patients were TST positive (36%). IGRA was performed on 203 patients with a positive TST, and 110 were IGRA positive (54%). In total, 151 patients were eligible for LTBI treatment, and 147 were offered treatment. Of those, 141 (96%) agreed to start treatment and 103 (73%) completed an entire course of LTBI treatment. There was a significant correlation between non-adherence to therapy and young age, and being of Sub- Saharan African origin. The authors conclude that earlier integration of LTBI screening into refugees’ medical care can result in very high proportions of patient retention as well as excellent proportions of acceptance and completion of LTBI treatment. They state that a systematic program of screening and treatment of LTBI in refugees as part of a comprehensive refugee clinic is feasible and effective (10).
Study 2, from Subedi et al. (11), a retrospective cohort study from 2015, compared LTBI screening and treatment of refugees between two different groups of facilities: Philadelphia Refugee Health Collaborative (PRHC) facilities and non-PRHC facilities. The authors found that patients treated at PRHC facilities were nine times more likely to complete LTBI treatment than patients treated at non-PRHC facilities. The PRHC facilities are staffed by physicians with special expertise in primary care for new immigrants. Refugees seen at PRHC clinics were more likely to be screened within 30 days of arrival (OR 4.70, 95%CI 2.12– 10.44), attend a follow-up appointment (OR 4.53, 95%CI 1.36–16.27), or complete treatment (OR 9.44, 95%CI 2.39–37.30), as compared to those seen at non-PRHC clinics. The PRHC clinic model offers a multidisciplinary approach whereby doctors, nurses, social workers and case workers from both the volunteer agencies and the Philadelphia Department of Public Health (PDPH) manage the screening, evaluation and treatment follow-up of the refugees (11).
In contrast, in a different population and setting, study 3 from Rubinowicz et al. in 2014 (12) evaluated the role of primary care physicians in the treatment of LTBI in Quebec among the general population. The authors found that 37% of patients who were prescribed isoniazid (INH) for LTBI by primary care physicians completed treatment, as opposed to 42% of those prescribed by other physicians (p < 0.0001). Patients dispensed INH initiated by primary care physicians were significantly less likely to complete treatment (OR 0.8, 95%CI 0.72-0.86). As well as the specialty of the prescribing physician, the authors found that sex and age increased the likelihood of treatment completion, with middle age and older men (50-75 years) being most likely to complete treatment. The authors could not determine the type of institution where the prescriber worked, which could be an important factor in their results; some physicians work alone, while others work with teams and specialists. The reasons why completion was less likely among those prescribed by primary care physicians remains unclear (12).
Study 4, from Tavitian et al. published in 2003, describes a pharmacist-managed clinic for LTBI treatment in Health Care Workers (HCW), achieving LTBI treatment completion rates higher than 90% (13). Before 1993 LTBI treatment completion by HCW at Cedars-Sinai Medical Center in Los Angeles was very low (under 1%). The LTBI clinic was created as an extension of the employee health service (EHS), staffed by a pharmacist, a medical resident, and a nurse. During the first study period (retrospective) 158 HCWs were referred to the clinic, 131 started LTBI treatment, 122 (93%) completed the recommended treatment. During the second study period (prospective) 183 HCWs were referred to the clinic, 163 started INH therapy, treatment completion for July 1997 to June 1998 was 90%, July 1998 to June 1999 94%, July 1999 to June 2000 100%, and July 2000 to June 2001 93%. The authors concluded that a pharmacist-managed clinic can enhance adherence to LTBI treatment (13).
Study 5 from Ignotti et al. (14) involved the use of a registry of active TB cases diagnosed and treated in the city of Cáceres, Brazil, to analyze the effectiveness of the Tuberculosis Control Program at an established, centralized TB care provider (called a “referral center”) in comparison to Family Health Program (FHP) clinics that had been recently developed. The authors found that patients treated by the FHP had lower TB cure rates and were more likely to abandon treatment. Between 1999 and 2004, 333 cases of TB were diagnosed and treated. The patients presenting with pulmonary TB and treated via the FHP were 67% less likely to be submitted to sputum smear microscopy at the time of diagnosis and 68% less likely to be submitted to sputum smear microscopy prior to discharge than those who were treated at the referral center. The patients monitored via the FHP presented a 16.4% lower cure rate than did those treated at the referral center, as well as being more likely to abandon treatment (OR 2.93, 95%CI 1.15-7.46) or die (OR 5.71, 95%CI 1.85-18.1). The underperformance of the FHP were explained by the authors to be the result of high staff turnover rates (14).
Study 6 from Chung et al. (2007) (15), a population based cohort study based on medical record review in southern Taiwan, showed a higher TB treatment success rate at a Chest Specialty Hospital than at other medical centers, regional hospitals, and district hospitals/primary practitioner services (92.6% vs 65.2%, 63.9%, and 68.0%, respectively, p < 0.01 for all comparisons). Patients treated by pulmonologists and those treated at the Chest Specialty Hospital were significantly more likely to successfully complete treatment than those treated by non-pulmonologists or treated at other health care institutions (OR 1.74, 95%CI 1.08-2.97 and OR 4.58, 95%CI 1.58-13.23 respectively). As well, patients treated by pulmonologists at the Chest Specialty Hospital had a higher successful treatment rate than those who were treated by pulmonologists at other institutions. The higher likelihood of success by pulmonologists at the Chest Specialty Hospital remained after adjusting for age and gender (OR 4.23, 95%CI 1.45-12.40). The authors attributed these differences to the specialist physicians’ expertise with the disease and a more efficient diagnostic and treatment process. Together, these results indicate that both the training of care providers and aspects of the institution providing care are important factors affecting the quality of TB care (15).
Study 7 from El-Sadr et al. (1996) (16) describes the experience of Directly Observed Therapy (DOT) implementation under a surrogate family model at The Harlem Hospital in New York, United States. The investigators found TB treatment completion rates higher than 85% under the Harlem program. The patient-centered program was designed to develop a sense of family among the program staff and the patients. This included on-site treatment supervision with home visits limited to homebound patients and to patients who missed visits; group activities; and the provision of incentives and supportive services. During the study period, 145 patients with confirmed or suspected TB were enrolled in DOT. Among all enrolled patients, 57.9% were HIV infected. The mean visit adherence rate was 91.1 ± 7.9% (median = 92%). A visit adherence rate of 80% or greater was achieved among 94.6% of patients, and 57.9% had a rate of 90% or greater. Of the 95 patients with confirmed TB, 84 completed the treatment (88.4%). The authors state that through a multifaceted approach and a uniquely supportive environment, the Harlem DOT program achieved high completion rates among an inner-city patient population, with a loss-to-follow-up rate of only 1% (16).
Three of the seven papers presented above exhibited results in favour of specialist driven LTBI treatment or a centralized model of TB care (12,14,15). Some of the explanations offered for this difference include political and program management issues rather than to differences in physician training. For example, in the study of the Family Health Program in Brazil (14), some of the contributing factors included the short term placements of program personnel, and inconstancy of the program. In contrast, four studies (one Canadian) concluded that primary care in an integrated TB program model can be better at achieving good treatment acceptance and completion rates (10,11,13,16). These models attributed their success to various factors, including the application of non-physician (e.g. pharmacist) managed programs, multidisciplinary teams, interpreter services, patient centered programs, active follow up of patients, incentives for patients, cultural approaches, and diverse educational approaches, among others.
3.2. Summary from BridgeCare Clinic Interviews and Program Data
3.2.1. LTBI Program and Care Pathway at BridgeCare Clinic
BridgeCare Clinic opened in 2010 as a refugee clinic. The clinic provides comprehensive primary care for government-assisted refugees during their first year in Winnipeg. Currently, the staff is comprised of one full-time primary care physician, one full-time nurse practitioner, one full-time primary care nurse, a community health worker and two primary care assistants. The facility has two exam rooms, one consult room, one staff room and a laboratory.
There are approximately 500 refugee clients at BridgeCare Clinic each year from various regions, including the Middle East (Syria), Horn of Africa (Somalia, Eritrea, Ethiopia), Sub- Saharan Africa (Congo) and Southeast Asia (Myanmar). Government-assisted refugees are referred to BridgeCare Clinic by two settlement agencies, Welcome Place and Accueil Francophone (each provides transition housing services for refugees in Winnipeg). Refugees are eligible to receive health care at BridgeCare Clinic during their first year in Canada, after which they are referred to other community health care clinics.
Basic medical screening is offered to refugees within two weeks of their arrival to Canada. The primary care nurse at BridgeCare Clinic receives the referrals from the settlement agencies. The referral includes the country of origin and other countries that the individual had visited before their arrival to Canada. Based on this history, individuals between 18 and 49 years of age may be eligible for LTBI screening and management as a part of their intake process. Refugees from a TB endemic country, defined as a country experiencing more than 30 cases of TB per 100,000 people every year, are eligible (7). The majority of refugees that need screening for LTBI at BridgeCare Clinic have arrived from countries in Africa. Refugee children are also seen at the clinic, but are not screened for LTBI.
LTBI screening and management are performed following the guidance of the Canadian Tuberculosis Standards (7) and the Practice Guideline Process for Monitoring INH administration in Adults Being Treated for LTBI (Adult) from the WRHA (17).
All clients have an initial intake appointment with a primary care nurse and an outreach worker, followed by a further visit in follow-up with a physician or nurse practitioner. Interpreter services, funded by the WRHA, are available during assessments.
In 2013, BridgeCare Clinic began a pilot project to offer to adults aged 18 to 49 years free screening for LTBI with TST and IGRA. If a TST was positive, an IGRA test was performed. After finding significant challenges with the use of TST requiring a total of up to 4 visits to the clinic, a switch from a combined TST/IGRA approach to the sole use of IGRA testing was implemented for LTBI screening in 2014. IGRA was provided at no cost for clients through an in-kind contribution from Cadham Provincial Laboratory where the tests were performed.
Figure 2 describes the typical care pathway for LTBI in adults at BridgeCare Clinic. A few weeks after the first appointment, a follow-up visit with a physician or nurse practitioner is scheduled. This visit includes a complete physical examination and review of the blood test results. If the IGRA test is positive, the physician or nurse practitioner inform the client of the result and discuss LTBI, including the natural history, transmission and management options.
Additionally, the physician or nurse practitioner order a chest X-ray to rule out active TB. The X-rays are performed at the Health Sciences Centre General Hospital or at Manitoba Clinic. If their chest X-ray is normal, and they are eligible for LTBI treatment, INH treatment for nine months is offered. If there is any evidence of liver dysfunction, treatment with rifampin (RIF) for four months is discussed.
The eligibility criteria for LTBI treatment include:
- Not being pregnant;
- Not being on a medication that is incompatible with INH;
- Not having a medical condition that would contraindicate taking INH (i.e. chronic hepatitis B, severe elevation of baseline ALT); and
- Not having a condition that predicts non-adherence (i.e. untreated mental health disorder, memory issues, etc.).
Education is a very important part of the process for LTBI management at BridgeCare Clinic. At the time of medication initiation, the primary care nurse explains to the client the difference between active and latent TB, the natural history of LTBI, management of LTBI including medications and potential side effects, the need for contraception in women, adherence, and the importance of minimizing the use of other potential hepatotoxins such as alcohol and Tylenol.
Pregnant women are screened for LTBI but treatment is deferred until three months postpartum. At the end of the 12 month period when clients are referred to another clinic for ongoing primary care, the LTBI screening results are also transferred.
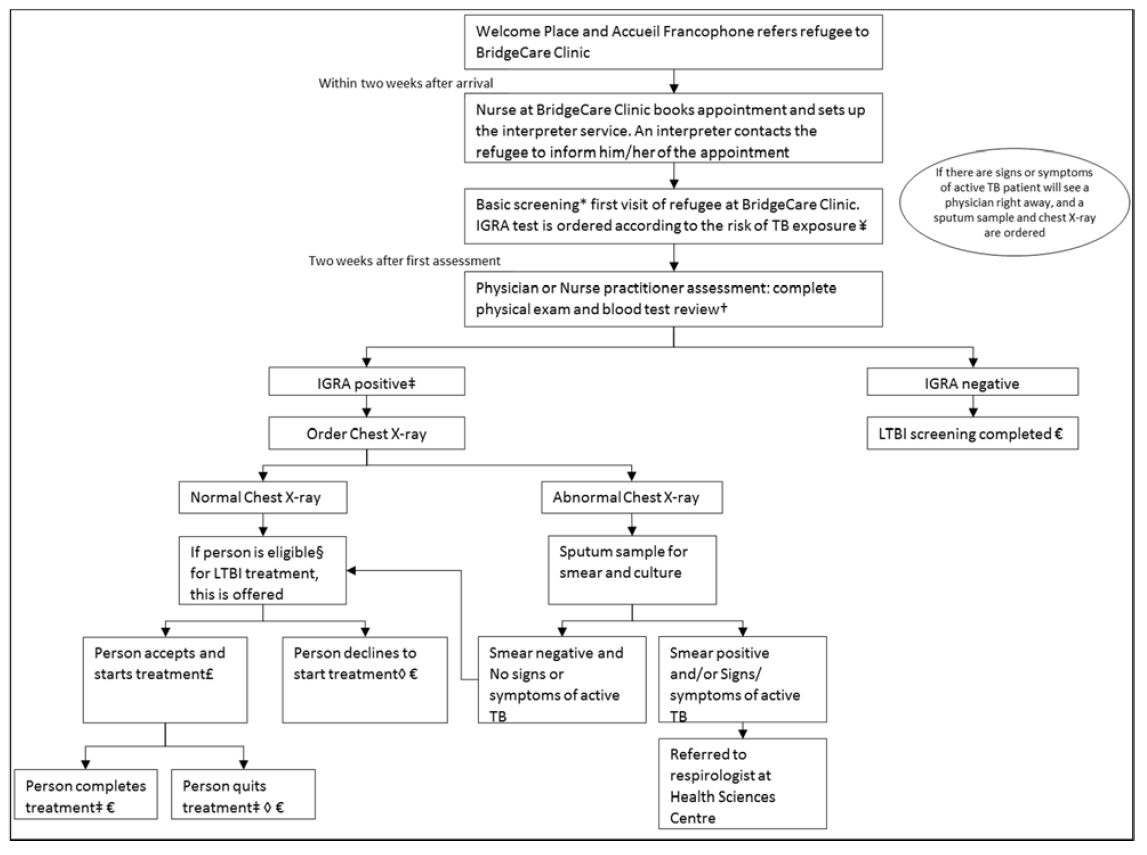
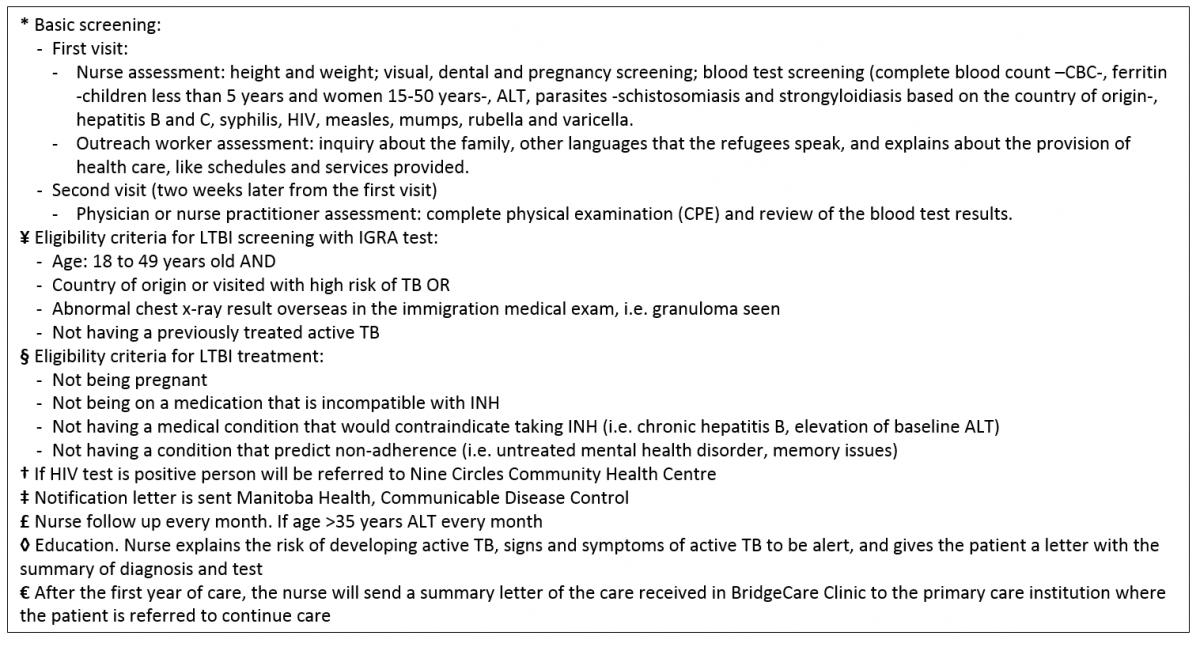
Figure 2. Typical care pathway for latent tuberculosis infection at BridgeCare Clinic.
A stock medication supply is available at BridgeCare Clinic in case clients want to start on treatment during their initial intake; their first package is taken from the stock and the prescription is then backfilled. There is no cost to BridgeCare Clinic, or to the client. The medication is usually dispensed in a blister pack for 28 days (Figure 3). Clients are followed monthly, with visits scheduled by the primary care nurse and recorded on a card that the client keeps. Clients also receive pamphlets in their own language with information on the definition of LTBI, why to treat LTBI, how to take INH and INH side effects. The prescription is sent to the pharmacy for future dispensing. Finally, the nurse also sends a summarized letter to Manitoba Health, Communicable Disease control.
If someone declines treatment, the primary care nurse will provide them with information about the signs and symptoms of active TB. Clients will also receive a letter from the primary care nurse with the same information and their test results are sent to their home.
Monitoring for side effects is a routine part of follow-up. During the treatment course, if the client is older than 35 years, an ALT is done monthly. If the client is younger than 35 years the ALT is performed only if symptoms or signs of hepatotoxicity are present.
Clients who want to discontinue treatment are counselled by the primary care nurse on the importance of adherence and possible reasons for discontinuing are explored. Clients are encouraged to complete at least six months of INH treatment. If clients discontinue treatment, they receive documentation regarding their LTBI diagnosis and treatment, as well as information on the signs and symptoms of active TB. Finally, a letter is sent to Manitoba Health, Communicable Disease control.
Upon completion of treatment, clients receive a letter with the treatment course identifying that treatment is complete and a letter is also sent to Manitoba Health, Communicable Disease control.
When clients miss a follow-up appointment, the clinic staff calls them to set up a new appointment. In the case of a client who moves to another province, BridgeCare Clinic notifies Manitoba Health, Communicable Disease Control, and it will notify the RHA in the client’s new province in order for them to resume LTBI treatment there.

Figure 3. Blister pack for 28 days of isoniazid and pyridoxine for LTBI treatment
When a baseline chest X-ray is abnormal, active TB is ruled out with a history and sputum culture. If the smear/culture is negative and the client is asymptomatic, they are offered LTBI treatment. Clients with active TB are referred to the respirologist at Health Sciences Centre Hospital.
HIV testing is performed routinely as part of the general assessment at baseline. Clients with a positive HIV test are sent to Nine Circles Community Health Centre for management of their HIV. In these instances, the client’s LTBI is also managed through Nine Circles Community Health Centre.
3.2.2. Facilitators and Barriers for LTBI Care
The facilitators and barriers for LTBI care identified at BridgeCare Clinic through interviews have been categorized according to the five levels of the social ecological model (SEM) proposed by McLeroy and colleagues (18) and updated by Kumar and colleagues (19) and McClarty and colleagues (20,21). The social ecological model arose in the context of health promotion, in an attempt to understand how health is influenced not only by human behavior but also by environment and social structures (18). The levels included in the model are: the intrapersonal level, the interpersonal level, the institutional level, the socio-cultural/community level, and the structural/policy level.
The intrapersonal level comprises characteristics of the individual (e.g. knowledge, behavior, self-concept, etc.). The interpersonal level includes social networks and social support systems (e.g. family, work group, and friendship networks). At the institutional level social institutions are included, such as health care organizations. The socio-cultural/community level consists of relationships among organizations, institutions, and also cultural norms. Finally the structural/policy level incorporates policies at all levels (18–21).
A description of the facilitators and barriers identified by staff and organized by level of the SEM model is provided below and summarized in Figures 4 and 5 respectively. Interpretations, as described below, are supported by references to clinical guidelines and peer reviewed literature.
Facilitators
Intrapersonal level
Interviewed staff identified the following as facilitators at the intrapersonal level:
The absence of side effects with first line treatment. A common side effect of INH is an upset stomach. Adherence to INH is even more likely if this relatively mild side effect is not present (22).
The low prevalence of alcohol dependence/issues among refugee populations. INH can cause liver toxicity. It is therefore recommended that individuals taking INH avoid alcohol intake. If a patient cannot stop their alcohol consumption during treatment, INH should not be initiated. As well, alcohol dependence/issues often result in low treatment adherence (23,24). Alcohol dependence/issues have been very rare among the refugees seen at BridgeCare Clinic (25).
Interpersonal level
Strong relationships with clients: The relationships established between health care providers and clients help to promote treatment compliance. At BridgeCare Clinic, clients receive integrated health care; health care providers can therefore establish a strong relationship with clients through various visits for multiple purposes, including physical examinations and vaccine catch up.
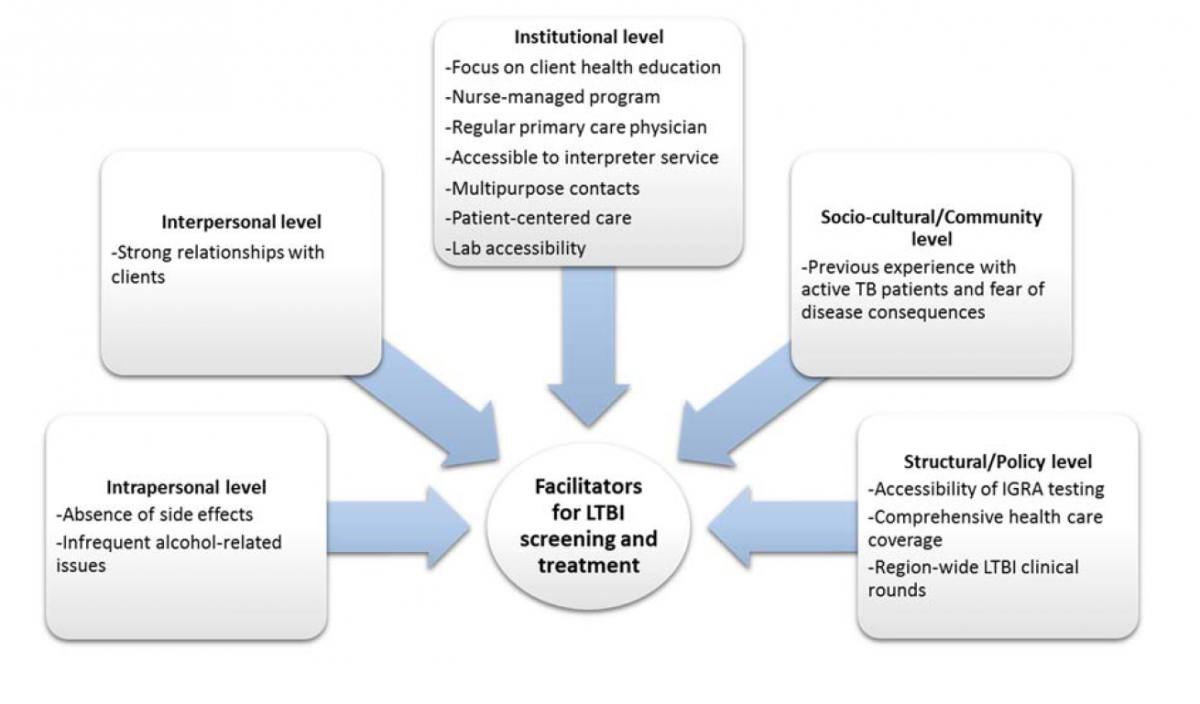
Figure 4. Facilitators for latent tuberculosis infection screening and treatment at BridgeCare Clinic reported by interview participants.
Institutional level
A significant focus on client health education. Health education can help increase treatment adherence (26). At BridgeCare Clinic, health education is provided over multiple encounters with clients, so that information is consistently reinforced. Clients receive health education from both physicians and nurses, and written information is also provided.
Nurses in central program management roles. The LTBI program at BridgeCare Clinic is a nurse run program. The program is therefore strongly influenced by nursing care models which tend to emphasize a holistic approach to disease, and focuses on the changing needs and situation of each individual patient.
Clients assigned to a regular primary care physician. At BridgeCare Clinic, clients are assigned to a physician and receive integrated primary health care with their LTBI care. Physicians are therefore involved in the complete care of clients, including other screening and health services. This relationship facilitates better LTBI treatment completion outcomes than systems where clients receive partial and ephemeral care from multiple health care providers (27–29).
Accessible and well utilized interpreter service. Communication is fundamental for health care and attaining successful treatment completion outcomes. The BridgeCare Clinic regularly utilizes an interpreter service offered by the WRHA to communicate and educate refugees who speak different languages.
Multipurpose contacts with clients. The provision of LTBI care within a primary health care setting results in multipurpose contacts with clients. This provides the opportunity to enhance LTBI education, alleviate concerns, and improve treatment adherence.
A patient-centered approach to care. The staff at BridgeCare Clinic actively follow all individuals receiving care at the clinic. They try to establish good relationships with clients by taking into account their personal needs. This includes access to interpreter services, the provision of health education, and the provision of primary health care to clients’ families, which stimulates family involvement.
Improved efficiency and accessibility of laboratory services. Laboratory sampling in BridgeCare Clinic was opened in January 2016. Prior to this, lab accessibility was limited, and BridgeCare Clinic staff encountered challenges trying to align patient blood sampling for IGRA with restricted hours of lab availability. Clients also had to go to Health Sciences Centre, a tertiary care centre, for their lab work and sometimes encountered language barriers. As a result, there were many canceled and rescheduled IGRA tests before laboratory sampling was available at the clinic. Integration of the lab enables a “One Stop Shop” approach.
Socio‐cultural/Community level
Increased likelihood of refugees having personal experience with active TB patients and fearing disease consequences. Individuals under LTBI screening at BridgeCare Clinic were either born in, or visited, a high TB burden country. This increased their likelihood of knowing persons with active TB, and witnessing some of the suffering caused by the disease, including death. These experiences contribute to their fear of the disease and their willingness to start and complete treatment.
Structural/Policy level
The availability and accessibility of IGRA testing. Under the in-kind provision of Cadham Provincial Laboratory, IGRA testing is available for refugees at BridgeCare Clinic. According to the literature, IGRA performs better than TST among certain populations like refugees (30). Advantages to IGRA include: the need for only one visit for blood sampling, with a significantly wider period of time for sampling during the week (rather than two visits for a TST application and reading, with limited time and days for sampling); IGRA testing has higher specificity, especially in individuals previously vaccinated with BCG (increased likelihood in refugee populations); IGRA test interpretation is systematic and does not involve as many subjective steps as TST. Staff at BridgeCare Clinic found IGRA to be more convenient, effective, and easier to interpret than TST.
Comprehensive health care coverage for refugees (during first year in Canada). Government-assisted refugees can receive comprehensive health care at BridgeCare Clinic during their first year in Canada at zero cost to them. This includes basic screening (figure 3), outreach worker supports, and vaccine catch up, among others.
Region-wide clinical rounds specific to LTBI. ITBS rounds are monthly meetings chaired by WRHA-ITBS leadership to discuss TB/LTBI client scenarios in order to support clinician decision making, communication and application of guidelines. They also present opportunities for discussion about system improvement. BridgeCare Clinic staff regularly attend this meeting and have the opportunity to discuss challenging LTBI cases with colleagues and experts, as well as be updated on emerging research and practices.
Barriers
Intrapersonal level
Younger age of some clients. Younger age can be a barrier for LTBI treatment. In the experience of BridgeCare Clinic staff, younger clients find it more difficult to understand the need for medication when they feel well. Younger, school-age clients present a greater challenge due to their desire to not miss classes or alter their school schedules for appointments. Nurses at BridgeCare Clinic try to accommodate their schedules by providing them late appointments in the day.
Concern regarding side effects. Concern about side effects can be another barrier for treatment acceptance. Although there are some described side effects related to LTBI treatment, the concern among clients is often disproportionate to the documented risk of side effects.
Low health literacy among some clients. There is a wide spectrum of literacy among BridgeCare Clinic clients. When health literacy is low, it is more difficult for staff to explain important health concepts such as the meaning of LTBI, and the difference between LTBI and active disease.
Language barriers. Even with the interpreter service, language still can be an issue. For some languages it is very difficult to find a direct interpreter, which can affect communication with the client.
Unknown age. Clients at BridgeCare Clinic may not know their own age which has implications on their eligibility criteria for LTBI screening.
Unknown medical history. A very challenging issue with refugee populations can be establishing if they have received active TB treatment in the past. At BridgeCare, this is asked three times: in the first assessment by the primary care nurse, during the physical evaluation by the physician or nurse practitioner, and during the appointment to start LTBI treatment. However, sometimes it is still very difficult to know for certain.
Pregnancy and family planning. Although INH can be taken during pregnancy, in pregnant women there is still concern of side effects to the fetus and hepatotoxicity to the woman. In pregnant women at BridgeCare Clinic LTBI treatment is deferred until three months postpartum. For those planning to get pregnant, LTBI treatment is discussed and the client can decide whether to start treatment or not. Contraception is offered to all women to avoid pregnancy during treatment. This can be a barrier to treatment if women do not want to use contraception.
Long duration of first line treatment (INH). The nine month course of INH is perceived to be very long for some clients and is a barrier to treatment acceptance and completion. There are current discussions at BridgeCare Clinic around offering alternative shorter-course treatments (e.g. four months of rifampin) Interpersonal level During the analysis of the orientation and interviews, interpersonal level barriers were not identified.
Institutional level
Laboratory service availability. Despite improvements in laboratory services accessibility, there are still limits to the days and times when blood sampling for IGRA tests can occur. This is primarily due to the availability of the referral lab and technical issues inherent to the test.
Staff and resource limitations. As a comprehensive refugee clinic, resource limitations are always an issue. The availability of staff to respond in a timely manner to patient needs is related to the number of government-assisted refugees regularly arriving in Winnipeg. Until recently, the staff at BridgeCare Clinic was sufficient to serve approximately 500 people each year, without screening children for LTBI. In 2016, the budget was increased to serve approximately 650 clients per year, but with recent increases in refugee arrivals in the province, staff time and resources are still stretched. Resource limitations has also prohibited the inclusion of services such as screening for children, and dedicated LTBI program follow-up calls.
Communication across facilities and between providers. Pre-immigration chest X-ray results are not available for BridgeCare Clinic staff. In the case that a person has an abnormal pre-immigration chest X-ray (except those consistent with active TB) a respirologist at a Tertiary Care Hospital receives a letter from the Public Health Agency of Canada, and a similar letter is given to the assessed person. Communication gaps or errors can occur when another provider or the person with the abnormal chest X-ray result do not inform BridgeCare Clinic staff of the situation. This may result in a duplication of services.
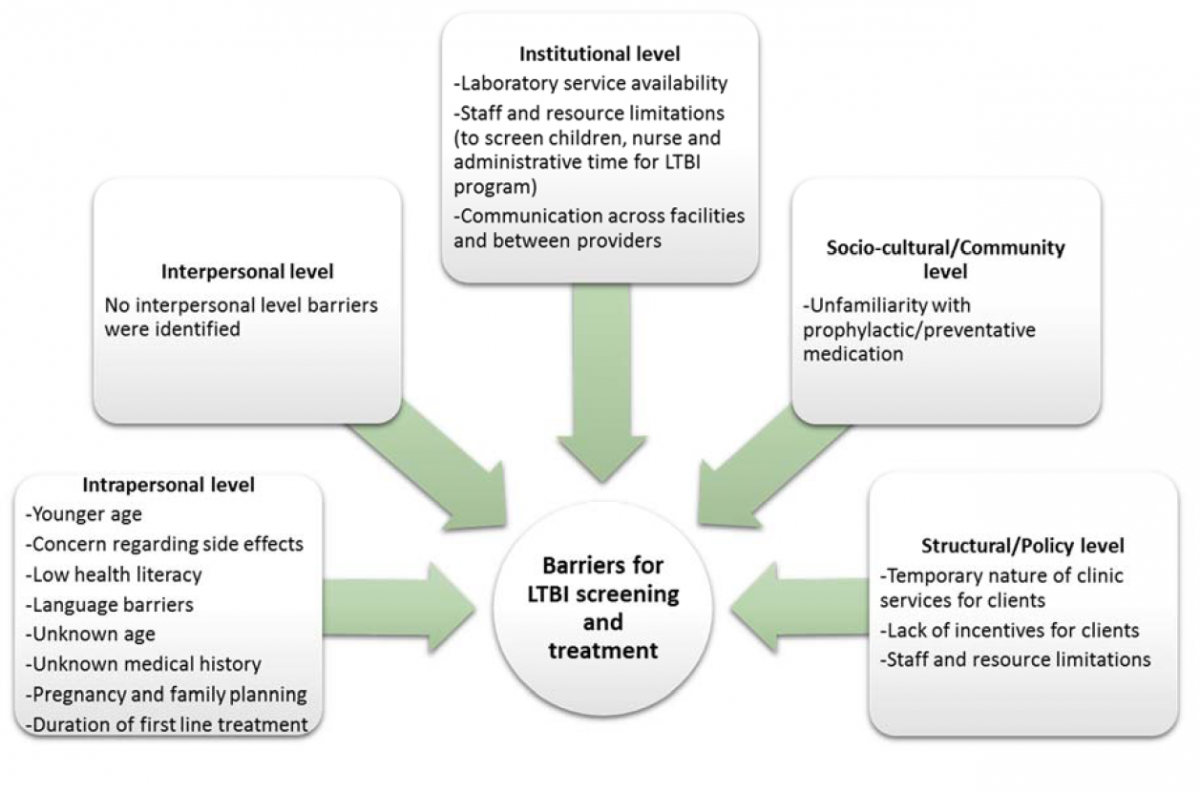
Figure 5. Barriers for latent tuberculosis infection screening and treatment at BridgeCare Clinic reported by interview participants.
Socio‐cultural/Community level
Unfamiliarity with prophylactic/preventative medication. The concept of taking medication for the purpose of prevention is not a familiar one among many refugee clients at BridgeCare Clinic. This could be due to cultural factors and/or the rarity of prophylactic/preventive medication in many of the countries where refugees are from. This unfamiliarity can affect LTBI acceptance rates, as clients may not understand why they should take medication when they do not feel sick.
Structural/Policy level
Temporary nature of clinic services for clients (1 year duration). Health care provision for refugees at BridgeCare Clinic ends approximately after the first year of arrival to Canada. At that time, clients are referred to a different primary care clinic for their health care needs. This presents some challenges to clients trying to complete the LTBI screening and treatment process before they move to another clinic and potentially compromise their continuity of care (especially with a nine month INH regimen).
Lack of material incentives for clients to complete treatment. Evidence indicates that the provision of incentives to individuals requiring treatment for active TB or LTBI—for instance foods, money, celebrations, etc.—enhance treatment acceptance and completion rates (31–33). As these incentives require additional funding, there is currently insufficient resources to support this kind of strategy, not only at BridgeCare Clinic, but also in TB prevention at the national level.
Staff and resource limitations. Staff and resource limitations can be a challenge at the structural/policy level in addition to the institutional level.
3.2.3. Summary of LTBI Program Data at BridgeCare Clinic
Between January 2015 and October 2016, 274 IGRA tests were ordered as part of the LTBI screening program at BridgeCare Clinic. IGRA results were negative in 158 clients (57.7%) and positive in 101 clients (36.9%). Of the remaining 15 tests: one result was deleted and one was referred due to other health conditions; five were cancelled by clients; one sample could not be processed and one result was indeterminate. Six tests were still pending at the moment of this report (Table 2).
The mean age of clients with a negative IGRA test result (29.6 years, SD: 8.8) was significantly lower than the mean age of clients with a positive IGRA test result by 2.9 years (32.5 years, SD: 8.9) (difference 2.9, 95%CI 0.682 – 5.118, p=0.005) (Table 2).
Similar sex distributions were seen between clients with a negative IGRA test result, and those with a positive test result. Out of 158 clients with a negative result, 71 were men (44.9%) and 87 were women (55.1%). Of the 101 clients with a positive result, 45 were men (44.6%) and 56 were women (55.4%). There was no significant difference between male and female proportions in either of the two groups (Table 2).
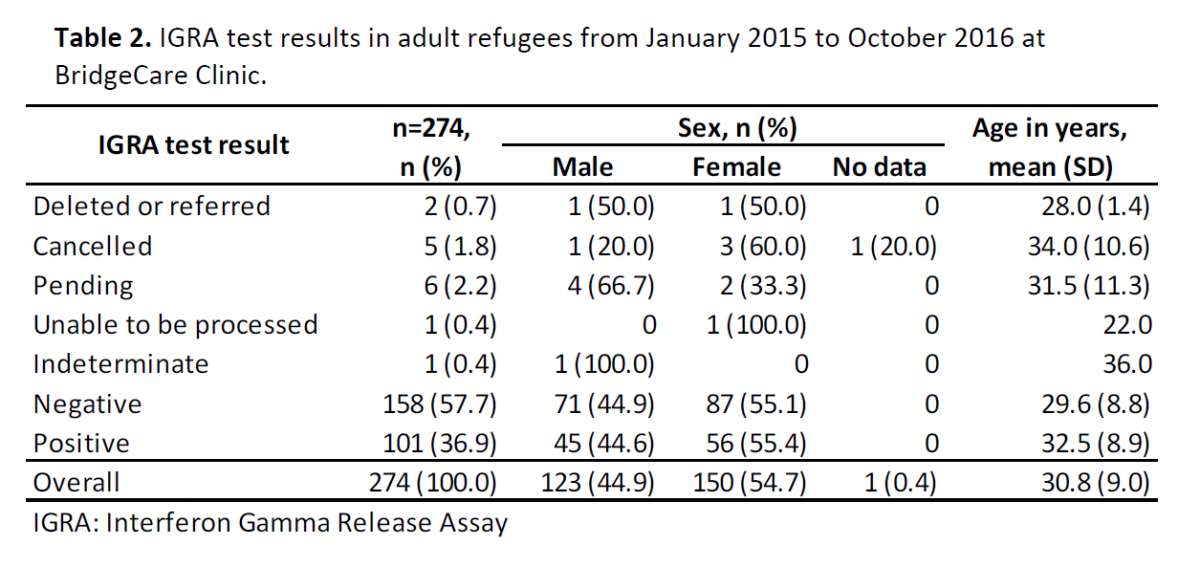
Table 2. IGRA test results in adult refugees from January 2015 to October 2016 at BridgeCare Clinic.
Clients from 23 different countries received an IGRA test at BridgeCare Clinic during the 22 month study period. People from four countries accounted for 60.2% of the BridgeCare Clinic clients: the Democratic Republic of the Congo (30.3%), Eritrea (17.5%), Burundi (6.2%) and Liberia (6.2%). If grouped by the WHO regions (34), 222 came from Africa (81.0%), 30 from Eastern Mediterranean (10.9%) and 20 from South East Asia (7.3%) (Table 3).
By WHO regions, 40.1% of the IGRA results for clients from Africa were positive, 23.3% for those from the Eastern Mediterranean were positive and 25% for those from South East Asia. The positive IGRA test result proportion in clients from the Eastern Mediterranean was 16.5% lower than the proportion from African clients (difference -0.165, 95%CI -0.332 – -0.003, p=0.038). Of the 101 clients with IGRA positive results, 89 (88.1%) came from an African country; this proportion was higher than the proportion of clients that came from African countries in the negative IGRA test result group (121; 76.6%) (difference 0.115, 95% CI 0.024 – 0.207, p=0.010) (Table 4).
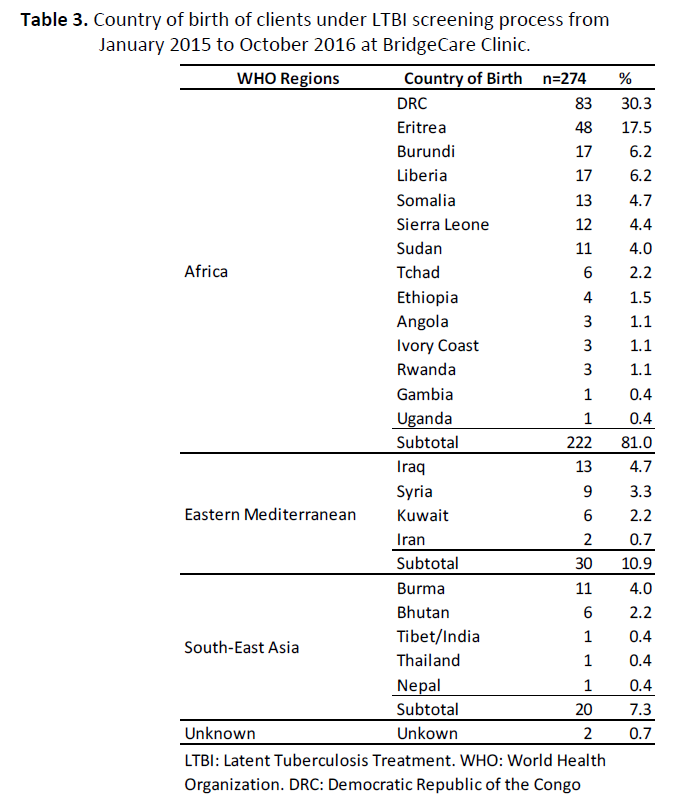
Table 3. Country of birth of clients under LTBI screening process from January 2015 to October 2016 at BridgeCare Clinic.
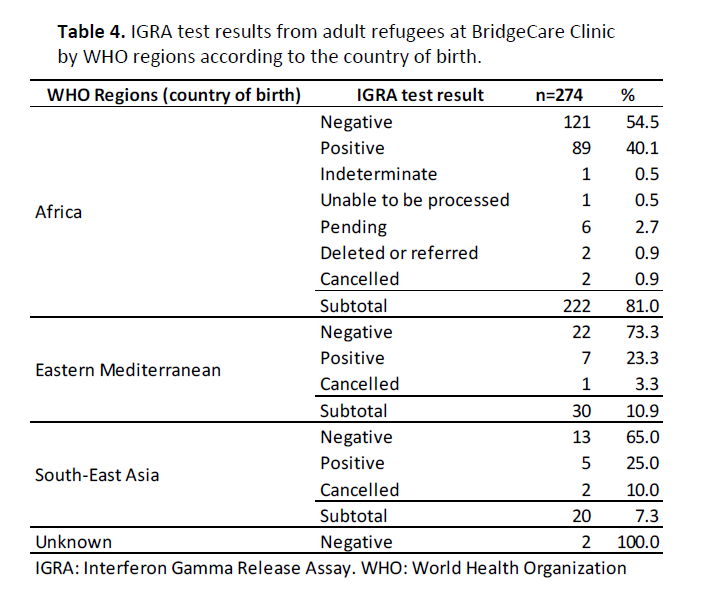
Table 4. IGRA test results from adult refugees at BridgeCare Clinic by WHO regions according to the country of birth.
LTBI treatment acceptance and completion rates were calculated using program data for January-December 2015. During this period 159 IGRA tests were ordered at BridgeCare Clinic, and 59 (33%) were positive.
Treatment Acceptance: Of 45 clients eligible for LTBI treatment, 10 (21.3%) declined to receive treatment, and 34 (75.6%) started treatment (Table 5).
Treatment Completion: Twenty seven (79.4%) clients completed treatment, 3 (8.8%) clients had moved out of province, and 4 (11.8%) quit treatment (Table 5).
Of the 28 women with IGRA positive results, 12 (42.9%) started treatment. This was significantly lower than the proportion of men that started treatment: 22 out of 31 (71%) (difference -0.281, 95%CI -0.524 – -0.038, p=0.015).
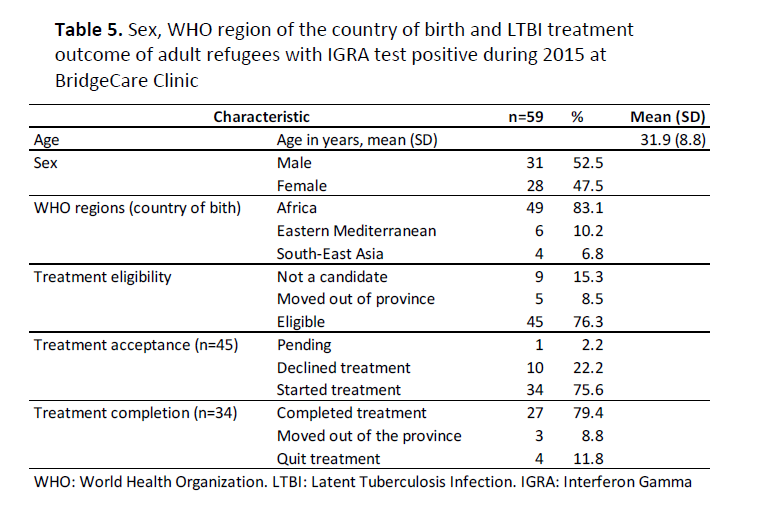
Table 5. Sex, WHO region of the country of birth and LTBI treatment outcome of adult refugees with IGRA test positive during 2015 at BridgeCare Clinic
3.3. LTBI Care Cascade for Refugees in Manitoba
To further support the analysis of LTBI care and treatment outcomes for priority populations under the TB management model of BridgeCare Clinic and WRHA-ITBS, the following LTBI care cascades for refugees in Manitoba (Figure 6) and refugees treated at BridgeCare Clinic (Figure 7) were created. The LTBI care cascades can help identify steps where losses of diagnosis and treatment occur for a particular population (35).
During 2015, Manitoba received 1767 refugees, with most (97%) moving to Winnipeg. Only a subset of these were classified as government-assisted refugees (694, 39.2%). While the majority of government-assisted refugees receive health care at BridgeCare Clinic, those who are French speaking receive health care at Centre de santé Saint-Boniface. (36)
Figure 6 demonstrates that among refugees in Manitoba, a major information gap exists regarding non-government-assisted (privately sponsored) refugees, as no data could be found on the LTBI screening process for this group. A large loss occurs between those initially assessed and those tested for LTBI. A large number of these individuals were not screened after initial assessment because they did not come from a high TB risk country; another large portion of this group includes refugee children, as they are currently not screened in Manitoba.
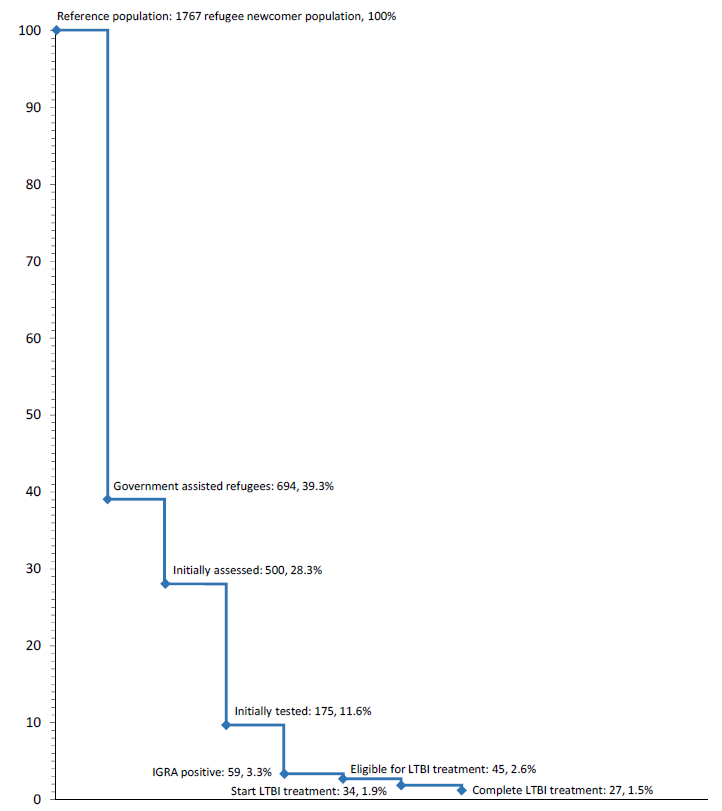
Figure 6. Losses in the cascade of latent tuberculosis infection care in refugee population in Manitoba.
The cascade of LTBI care at BridgeCare Clinic (Figure 7) demonstrates that even with good acceptance and completion rates (around 80%), a large proportion of losses to start treatment exists. Established reasons for these losses include movement from the province, fear of side effects, and pregnancy or plans for pregnancy, among others. Another proportion of losses occur because treatment that is initiated is not completed. The reasons for these losses include, again, movement from the province, and also factors such as the presence of side effects. An in-depth analysis of facilitators and barriers to treatment completion is found in section 3.2.2.
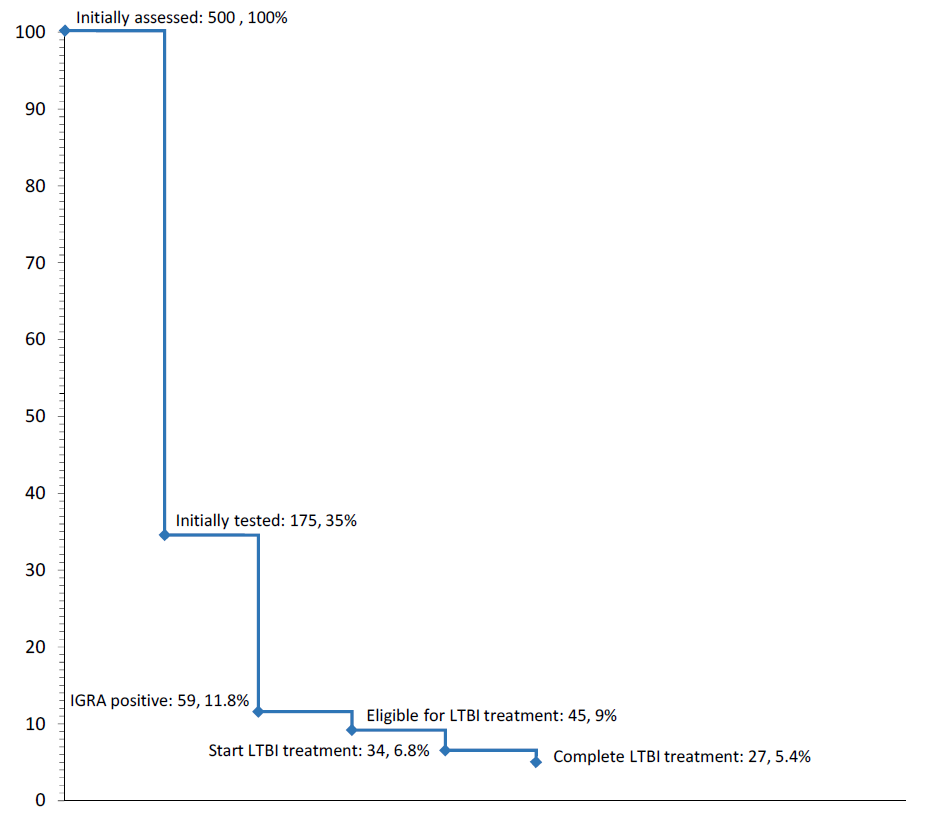
Figure 7. Losses in the cascade of latent tuberculosis infection care in refugee clients at BridgeCare Clinic.
Of those refugee clients at BridgeCare Clinic with positive IGRA and eligible for treatment, 24.4% decline treatment. The bottom of the cascade indicates that 60% of those eligible for LTBI treatment successfully complete treatment (Figure 8).
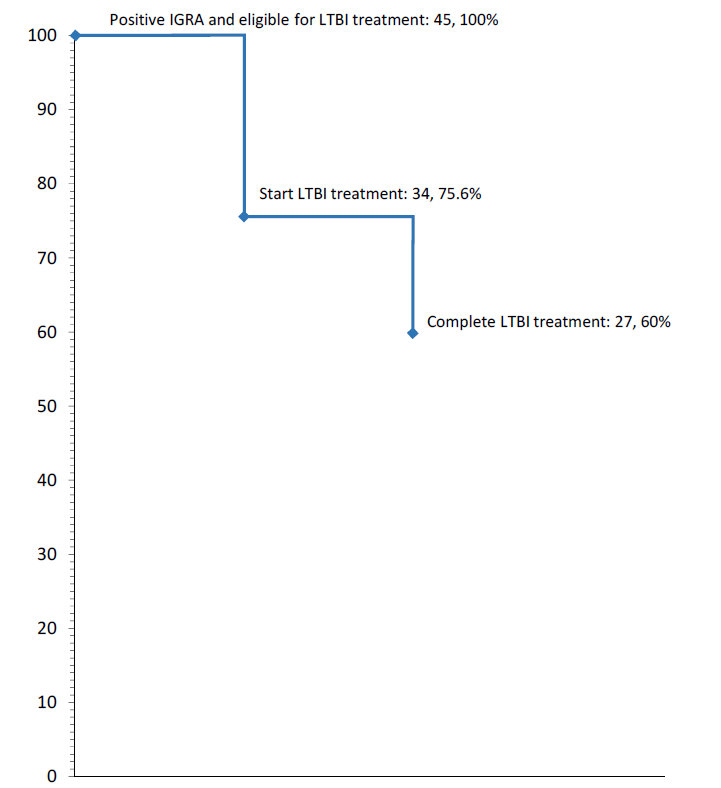
Figure 8. Losses in the cascade of latent tuberculosis infection care in refugee clients at BridgeCare Clinic with positive IGRA and eligible for treatment.
An analysis of LTBI treatment outcomes at BridgeCare Clinic in relation to those seen in other North American studies has demonstrated the clinic to be achieving good LTBI treatment acceptance and completion rates among its target population. A systematic review published in 2008 on adherence to LTBI treatment from the US and Canada describes completion rates among the foreign born population to range from 22% to 90%, depending on study size and type of population (37). In comparison, the present analysis of 2015 LTBI program data at BridgeCare Clinic revealed a treatment acceptance rate of approximately 76% and completion rate between 79% and 88% (upper estimate based on completion by those out of province). These estimates further validate findings by Manitoba Health, Seniors and Active Living, indicating promising treatment completion outcomes at primary care sites for noncomplex LTBI care (including BridgeCare Clinic) (5), and are very close to the 80% LTBI treatment acceptance and completion rate goals established by the Canadian Tuberculosis Standards (7).
A short review of the literature on treatment outcomes seen in comparable TB care settings and systems produced mixed findings. While the majority of reviewed studies produced evidence in support of program decentralization and the integration of TB management with primary care for priority populations, a number of studies displayed poorer treatment outcomes by such models. Authors attributed poor outcomes to factors that may have been specific to the particular centres being studied (e.g. personnel issues), but further research is required to assess what types of conditions spur success and what conditions produce challenges when integrating TB management with primary care. With this report, we begin to address these questions through our analysis of in-depth interviews and consultations with TB program staff at BridgeCare Clinic and the WRHA-ITBS.
The LTBI program at BridgeCare Clinic is an integrated program managed mainly by a primary care nurse. At this clinic, LTBI care is integrated with other care to the clients. According to BridgeCare Clinic staff, this is a very important characteristic of the clinic and is one of the central facilitators for successful LTBI screening and treatment. Integrated LTBI care with primary care can facilitate the initiation of multipurpose contacts with the patient and help develop strong relationships between the client and health care provider. The care model practiced at BridgeCare Clinic is patient centered and informed by a nursing care model. Staff from the clinic actively call and reach out to clients instead of waiting for clients to contact them. The outreach worker helps families learn how to navigate the health care system. The interpretation service contributes to a more culturally safe approach to care and improves communication between providers and clients. The education of clients also plays a very important role in TB management at BridgeCare Clinic. Finally, the availability of laboratory sampling at the clinic, free IGRA testing and efficient lab systems has contributed to treatment success at the clinic.
A number of barriers to successful LTBI treatment and care for refugees were also identified by the clinic staff. Many reflect those mentioned by the Pan-Canadian Public Health Network in their Guidance for Tuberculosis Prevention and Control Programs in Canada. These include barriers related to linguistic, cultural, socio-economic and health service gaps (6). While resource limitations can be seen as a challenge in any health program, recent increases in refugee arrivals to Manitoba has made dedicated staff time for LTBI management and lab accessibility for LTBI screening much scarcer.
Despite the effects of recent resource pressures, lab accessibility for BridgeCare Clinic clients was considered a significant facilitator for treatment acceptance and completion. This is due to the availability and coverage of IGRA for LTBI screening at the clinic; IGRA is not readily available for clients screened for LTBI outside of BridgeCare Clinic. It should also be noted that while the cost of TST is covered for those under TB contact investigation, other newcomers including refugees must pay for LTBI screening whether by TST or IGRA testing; however LTBI treatment is free. Only refugees assessed at BridgeCare Clinic therefore have access to free LTBI screening, creating an inequality in service.
LTBI treatment aims to reduce the risk of progressing to active TB, however according to previous studies the estimated number needed to treat to prevent 1 case of LTBI from progressing to active tuberculosis would range from 111 to 314 (depending on the patient’s risk for progression) (38), suggesting that the numbers that complete therapy through the program provided at BridgeCare Clinic may have limited impact on its own. LTBI care cascades presented in this report showed there is no information available about LTBI screening and treatment for approximately 60% of refugees arriving to Manitoba. In addition children are not screened for LTBI at BridgeCare Clinic, nor referred to another clinic for this purpose, and it is widely recognized that children especially under five years of age have higher risk of progressing from infection to active TB (7). The major gap is in entry to the program and narrowing of the gap for the remaining refugee population and increasing capacity may increase the number of individuals completing LTBI therapy and thus improve the impact of the integrated model. The limitation is the unavailability of data regarding the remaining 60% of refugees that do not receive services at BridgeCare Clinic.
The push towards integrated and decentralized TB care in Manitoba and Winnipeg appears to be consistent with global trends and guidance. In the most recent strategy for TB control by the WHO-The End TB Strategy, the organization calls for integrated, patient-centred care and prevention in TB programming. This means that the needs and expectations of patients must be systematically assessed and addressed. According to the WHO, this requires that all patients receive educational, emotional and economic support to empower them to complete the diagnostic process and full course of treatment. They suggest that National Tuberculosis Programs incorporate social support into clinical care and that treatment should include social protection measures and nutritional support (39). They emphasize that TB care, including ambulatory treatment should be decentralized, which would reduce the cost of treatment. Many of these recommendations align with the values and direction set out by the WRHA-ITBS in recent years. While focused on a particular population and health centre, this report further validates this movement and highlights areas where increased attention may be warranted.
It should be noted that many of the findings presented in this report were interpreted from information provided by BridgeCare Clinic staff. As no information was gathered from clients at the clinic, the description of facilitators and barriers to treatment and the LTBI care pathway are limited to only the staff’s perspective. Nevertheless, this model demonstrates the success of an inclusive model of care that can help to ensure that refugees with LTBI do not experience unnecessary challenges in their care.
References
1. Manitoba Health, Healthy Living and Seniors. Manitoba Tuberculosis Protocol. 2014.
2. Winnipeg Regional Health Authority. Care for All. Annual Report. 2014.
3. Winnipeg Regional Health Authority. Integrated Tuberculosis Services. Strategic Planning Workbook. 2012.
4. Winnipeg Regional Health Authority. WRHA Non complex LTBI Care Strategy within a Primary Health Care Intersectoral Model – Access Fort Garry and Nor’West – Non-complex LTBI assessment and management. Draft. 2016.
5. Manitoba Health, Healthy Living and Seniors. Distribution and Completion of Treated Latent Tuberculosis Infection in Winnipeg. Pre-release Report. 2016.
6. Pan-Canadian Public Health Network. Guidance for Tuberculosis Prevention and Control Programs in Canada. 2013.
7. Public Health Agency of Canada, The Lung Association, Canadian Thoracic Society. Canadian Tuberculosis Standards. 7th ed. Canada; 2014. 465 p.
8. Minister of Public Works and Government Services Canada. Tuberculosis in Canada 2014. Pre-release. Ottawa (Canada); 2016 p. 22.
9. Stop TB Partnership. High Burden Countries [Internet]. [cited 2016 Nov 9]. Available from: http://www.stoptb.org/countries/tbdata.asp
10. Rennert-May E, Hansen E, Zadeh T, Krinke V, Houston S, Cooper R. A Step toward Tuberculosis Elimination in a Low-Incidence Country: Successful Diagnosis and Treatment of Latent Tuberculosis Infection in a Refugee Clinic. Can Respir J. 2016;2016:7980869.
11. Subedi P, Drezner KA, Dogbey MC, Newbern EC, Yun K, Scott KC, et al. Evaluation of latent tuberculous infection and treatment completion for refugees in Philadelphia, PA, 2010-2012. Int J Tuberc Lung Dis. 2015 May;19(5):565–9.
12. Rubinowicz A, Bartlett G, MacGibbon B, Greenaway C, Ronald L, Munoz M, et al. Evaluating the role of primary care physicians in the treatment of latent tuberculosis: a population study. Int J Tuberc Lung Dis. 2014 Dec;18(12):1449–54.
13. Tavitian SM, Spalek VH, Bailey RP. A pharmacist-managed clinic for treatment of latent tuberculosis infection in health care workers. Am J Health Syst Pharm. 2003 Sep 15;60(18):1856–61.
14. Ignotti E, Oliveira BFA de, Hartwig S, Oliveira HC de, Scatena JHG. Analysis of the Tuberculosis Control Program in the city of Cáceres, Brazil, prior to and after the implementation of a Family Health Program. J Bras Pneumol. 2007 Jun;33(3):287–94.
15. Chung W-S, Chang R-E, Guo H-R. Variations of care quality for infectious pulmonary tuberculosis in Taiwan: a population based cohort study. BMC Public Health. 2007 Jun 11;7:107.
16. El-Sadr W, Medard F, Berthaud V. Directly observed therapy for tuberculosis: the Harlem Hospital experience, 1993. Am J Public Health. 1996 Aug;86(8):1146–9.
17. Winnipeg Regional Health Authority. Practice Guideline: Process for Monitoring INH administration in Adults Being Treated for LTBI (adult). 2015.
18. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Behav. 1988;15(4):351–377.
19. Kumar S, Quinn SC, Kim KH, Musa D, Hilyard KM, Freimuth VS. The social ecological model as a framework for determinants of 2009 H1N1 influenza vaccine uptake in the United States. Health Educ Behav. 2012 Apr;39(2):229–43.
20. McClarty LM, Lorway RR, Ramanaik S, Wylie J, Becker ML. Factors influencing frontline health service providersʼ likelihood to recommend a future, preventive HIV vaccine to key populations in Karnataka, south India. Vaccine. 2015 Jan 29;33(5):656–63.
21. McClarty LM. Potential barriers and facilitators to future HIV vaccine acceptability and uptake among marginalised communities in Karnataka, south India: perspectives of frontline health service providers. [Winnipeg, Manitoba]: University of Manitoba; 2013.
22. Denholm JT, McBryde ES, Eisen DP, Penington JS, Chen C, Street AC. Adverse effects of isoniazid preventative therapy for latent tuberculosis infection: a prospective cohort study. Drug Healthc Patient Saf. 2014;6:145–9.
23. Brudney K, Dobkin J. Resurgent Tuberculosis in New York City: Human Immunodeficiency Virus, Homelessness, and the Decline of Tuberculosis Control Programs. Am Rev Respir Dis. 1991 Oct 1;144(4):745–9.
24. Pablos-Méndez A, Knirsch CA, Barr RG, Lerner BH, Frieden TR. Nonadherence in tuberculosis treatment: predictors and consequences in New York City. Am J Med. 1997 Feb;102(2):164–70.
25. Beiser M. Health of immigrants and refugees in Canada, The (Commentary). Can J Public Health. 2005 Mar 1;96(2):30–44.
26. M’imunya JM, Kredo T, Volmink J. Patient education and counselling for promoting adherence to treatment for tuberculosis. Cochrane Database Syst Rev. 2012 May 16;(5):CD006591.
27. World Health Organization. Adherence to long-term therapies. Evidence for action. Geneva: World Health Organization; 2003. 196 p.
28. Centers for Disease Control and Prevention. Essential components of a tuberculosis prevention and control program. Recommendation of the Advisory Council for the Elimination of Tuberculosis. MMWR Recomm Rep. 1995;44(RR-11):1–16.
29. Centers for Disease Control and Prevention. Managing tuberculosis patients and improving adherence. Atlanta, Georgia: Centers for Disease Control and Prevention; 2014. 88 p.
30. Campbell JR, Krot J, Elwood K, Cook V, Marra F. A systematic review on TST and IGRA tests used for diagnosis of LTBI in immigrants. Mol Diagn Ther. 2015 Feb;19(1):9–24.
31. Lutge EE, Wiysonge CS, Knight SE, Volmink J. Material incentives and enablers in the management of tuberculosis. Cochrane Database Syst Rev. 2012 Jan 18;1:CD007952.
32. Beith A, Eichler R, Weil D. Worldwide: Incentives for tuberculosis diagnosis and treatment. In: Performance incentives for global health: potential and pitfalls. Washington, D.C: Center for Global Development; 2009. p. 237–56.
33. Centers for Disease Control and Prevention (CDC), New Jersey Medical School Global Tuberculosis Institute. Latent tuberculosis infection: a guide for primary health care providers. Atlanta, Georgia; 2013.
34. World Health Organization. Global tuberculosis report 2016. Geneva: World Health Organization; 2016. 192 p.
35. Alsdurf H, Hill PC, Matteelli A, Getahun H, Menzies D. The cascade of care in diagnosis and treatment of latent tuberculosis infection: a systematic review and meta-analysis. Lancet Infect Dis. 2016 Nov;16(11):1269–78.
36. Liz Robinson. Manitoba Immigration and Refugee Resettlement. Federal Ministerial Conference Discussing Impacts of TST/IGRA; 2016 Sep.
37. Hirsch-Moverman Y, Daftary A, Franks J, Colson PW. Adherence to treatment for latent tuberculosis infection: systematic review of studies in the US and Canada. Int J Tuberc Lung Dis. 2008 Nov;12(11):1235–54.
38. US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, Curry SJ, Bauman L, Davidson KW, et al. Screening for Latent Tuberculosis Infection in Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2016 Sep 6;316(9):962–9.
39. World Health Organization. Implementing the end TB strategy: the essentials. Geneva: World Health Organization; 2015. 113 p.
Annex 1.
Tuberculosis High Burden Countries (HBC) according to the World Health Organization
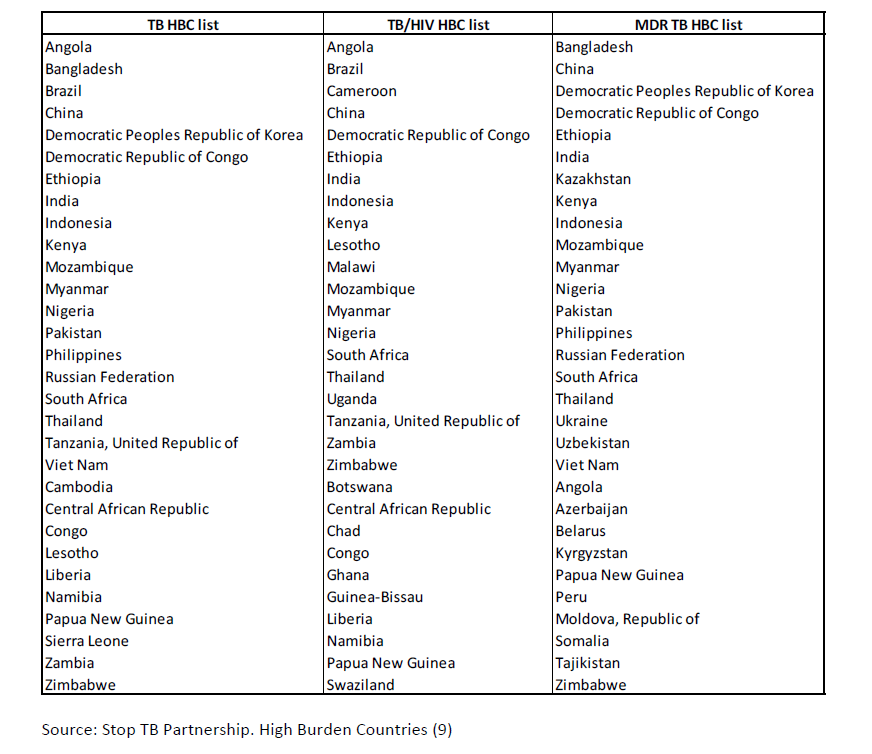
Source: Stop TB Partnership. High Burden Countries (9)
Annex 2. World Health Organization Regions
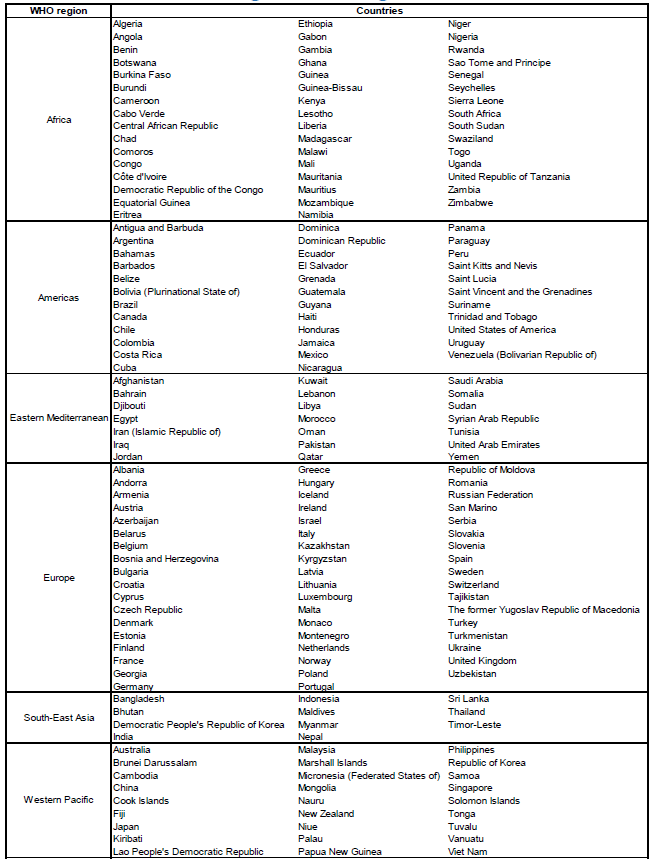
Source: http://www.who.int/about/regions/en/
Production of this document has been made possible through a financial contribution from the Public Health Agency of Canada through funding for the National Collaborating Centres for Public Health (NCCPH).
The views expressed herein do not necessarily represent the views of the Public Health Agency of Canada. Information contained in the document may be cited provided that the source is mentioned.
