Assessing the impact of varying levels of case detection and contact tracing on COVID-19 transmission in Canada during lifting of restrictive closures using a dynamic compartmental model
This study (with plain-language summary) underlines the importance of a cautious approach to lifting restrictive closures in this second phase of the epidemic. This approach includes efforts by public health to identify cases and trace contacts, and to encourage Canadians to get tested if they are at risk of having been infected and to maintain physical distancing in public areas.
Glossary of Terms
COVID-19 Modelling Glossary of Terms
Using and Understanding the Mathematical Model
1. To view and run this file, you will need the free version of RStudio, available here.
2. After downloading RStudio, download the following files:
3. Download the PHAC instruction guide:
Instructions for Using the COVID-19 PHAC Deterministic Compartmental Model
Model Description
This paper presents a mathematical research model developed by the Public Health Agency of Canada (PHAC) and Statistics Canada that assesses several non-pharmaceutical interventions (NPIs) on the SARS-CoV-2 pandemic on the attack rate of COVID-19 in Canada. The authors describe their simulations of the epidemic, the model parameters, simulations of NPIs, and their outcome measures. The authors emphasize the importance of creating age-stratified models to consider differences in contact and transmission rates, as there are few of them in the current literature. This model is an age-stratified, dynamic deterministic compartmental susceptible-exposed-infectious-recovered (SEIR) model. The results highlight the importance of detecting and isolating COVID-19 cases in addition to the tracing and quarantine of their contacts, for the control of the epidemic, in complement to physical distancing.
The model was implemented in RStudio and explored several NPIs, including case detection and isolation; contact tracing and quarantine; and changes to physical distancing as restrictive measures were lifted in May of 2020. The model equation includes compartments for hospitalizations, intensive care unit (ICU) admissions, including those on ventilators and also deaths. The transmission was measured using daily contact rates amongst and within six age groups. The assumptions of the model include:
- asymptomatic infectiousness is equal to that of symptomatic;
- all detected cases are isolated
- detection and isolation occur after the presymptomatic stage for each individual, and quarantining of contacts starts at the latent phase for each individual and covers the entire duration of its infectious period;
- quarantined individuals interact with only one person daily; and
- no births or non-COVID-19-related deaths occur in the population during the projected time.
The parameters and initializations of the model assumed community transmission began February 8, 2020 and parameter values were set according to an extensive review of the literature conducted by PHAC. The study design is for the entire population in Canada and included varying levels of case detection and isolation, contact tracing, and physical distancing from days 0-88 to fit observed cases.
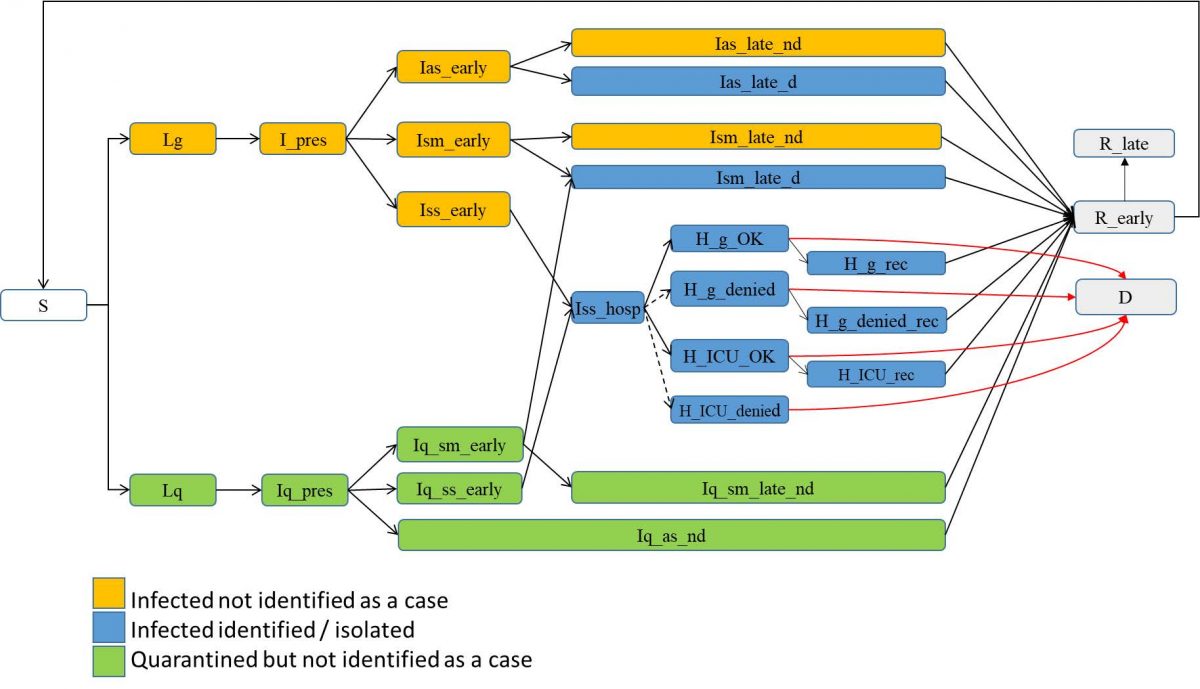
From day 88 (the date of lifting restrictive closures), there were three scenarios for physical distancing: i) contact rates remaining at 50% less than pre-COVID-19 levels (i.e., restrictive closures not lifted); ii) contact rates are allowed to increase up to 33% below pre-COVID-19 level; and iii) contact rates allowed to increase to 16.7% below pre-COVID-19 levels until the end of the simulation. Six levels of case detection/isolation (from 30% to 80% in 10% increments) and six levels of contact tracing/quarantine (from 30% to 80% by 10% increments) were simulated for each one of the three scenarios of physical distancing, for a total of 108 simulated epidemics.
The primary outcome was the number of infected Canadians over the 730 days and if the epidemic did not end (up to 2 years). Simulations over 730 days were not considered realistic due to the fact that recovered waning immunity was not modelled and individuals did not become susceptible again. The epidemic was considered controlled when the number of infected Canadians was under 10%.
Across simulations, the overall attack rate was found to be significantly worse when physical distancing was relaxed (1.6% -76.6% Canadians infected). The epidemic was controlled approximately 50% of the time when the contact rate was kept at half of pre-pandemic levels from day 88 forward.
Figure 1. Simulation of the epidemic for three scenarios after day 88 (May 4, 2020).
The y-axis includes all individuals in the infectious states—pre-symptomatic, symptomatic (hospitalized or not) and asymptomatic.
As an example, the epidemic was also controlled when 70% of cases were detected and isolated, coupled with 30% of contacts traced and half of the normal daily contact rate. Successfully detecting and isolating cases was found to be more effective then contact tracing but maximum efficiency comes from combining both.
This work highlights the importance of ensuring a relatively high level of detection/isolation of cases, and then, the tracing/quarantine of potentially infected cases, while maintaining some personal physical distancing to avoid a resurgence of the epidemic in Canada. For example, the total attack rate was lowest when these measures were effective at 80% of their capacity.
The model results are in accordance with models that are not stratified by age and can be applied nationally and locally. The model accounts for the main disease states, including latent and pre-symptomatic states, as well as the age structure in the Canadian population, which is important given that transmission varies by age. The model assessed case detection level rather than the ratio of asymptomatic cases, taking into account the current lack of precision on the number of asymptomatic cases, which is a still a challenge for COVID-19 modelling.
As with most mathematical modelling, translating the levels of NPI modelled into the real world is not always easy and can be open to interpretation. While the model uses current best estimates for parameter values, the values may change as knowledge of COVID-19 increases.
Current model (version 15)
Since the submission of the article describing the model, a number of modifications have been implemented to either add functionalities or allow the model to better account for more recent understanding of the COVID-19 transmission in Canada.
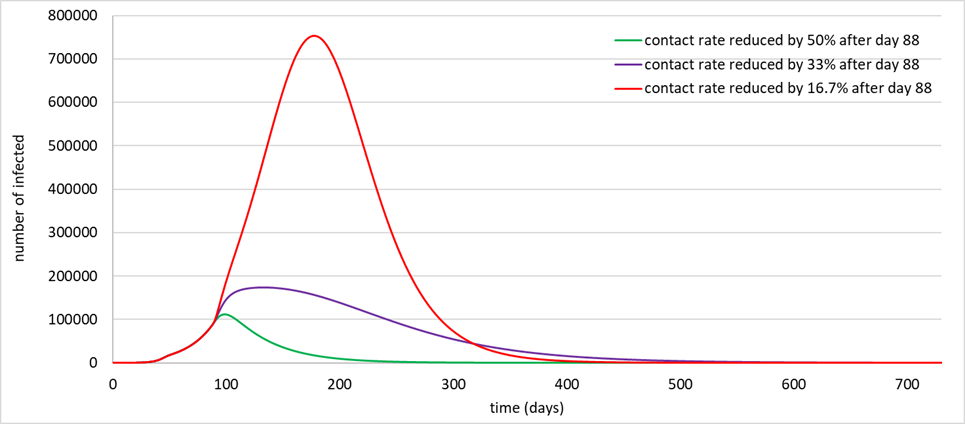
A more refined process of detection has been implemented to allow using specific detection/isolation capacity for asymptomatic, mildly symptomatic and severe symptomatic cases, both in the general population and in the quarantined population. The model now also provides the capacity to account for delays in getting isolated following onset of symptoms. This was implemented by dividing the symptomatic phase into an early and late phases where the early is used to account for delays, and do so in parallel for asymptomatic, mildly symptomatic and severe symptomatic cases. These compartment serve as a waiting chair until a case actually isolate itself.
Changes to the sections focusing on the hospital compartments were also made to allow for different occupation time for cases surviving the infection compared to those who don’t. Furthermore, a simplification was performed where cases requiring ventilator are now included in ICU units.
Finally, the capacity to simulate waning immunity has also been incorporated in the model.
The corresponding modified flux diagram can be seen in Figure 2 below.
Figure 2. Stocks and flow diagram of the PHAC SEIR model