Are you looking for the PHAC guidance document for practitioners?
NCCID Disease Debriefs provide Canadian public health practitioners and clinicians with up-to-date reviews of essential information on prominent infectious diseases for Canadian public health practice. While not a formal literature review, information is gathered from key sources including the Public Health Agency of Canada (PHAC), the USA Centers for Disease Control and Prevention (CDC), the World Health Organization (WHO) and peer reviewed literature.
This disease debrief was prepared by Ankita Mehra. Questions, comments, and suggestions regarding this disease brief are most welcome and can be sent to nccid@manitoba.ca.
What are Disease Debriefs? To find out more about how information is collected, see our page dedicated to the Disease Debriefs.
Questions Addressed in this debrief:
- What are important characteristics of Powassan Virus disease?
- What is happening with current outbreaks of Powassan Virus disease?
- What is the current risk for Canadians from Powassan Virus disease?
- What measures should be taken for a suspected Powassan disease case or contact?
What are important characteristics of Powassan Virus Disease?
Causes
Powassan virus is a tickborne flavivirus that causes Powassan disease. The pathogen is enveloped with a single-stranded positive sense RNA genome. The virus was named after Powassan, Ontario where it was first discovered in 1958. Two types of Powassan virus have been found in North America: Lineage 1 (prototype) and lineage 2 (deer tick virus) Powassan viruses. The 2 lineages are serologically indistinguishable and therefore the part of the same viral species.
Signs and Symptoms
Many people either develop mild, flu-like symptoms or no symptoms at all. The time from tick bite to developing symptoms ranges from 1 week to 1 month. Initial symptoms include fever, headache, vomiting, and weakness. More severe symptoms include confusion, loss of coordination, difficulty speaking, and seizures. In some individuals, it can cause a severe disease such as encephalitis or meningitis.
Severity and Complications
Powassan disease can be mild or severe. For people with more severe symptoms and disease, 1 out of 10 die. Approximately 10 percent of serious cases that develop encephalitis (inflammation of the brain) caused by Powassan virus are fatal and about half the people who survive the disease have long-term neurologic problems such as recurring headaches, muscle wasting, and memory problems.
Epidemiology
General
Powassan disease cases are rare, but infections are endemic in upper Midwest of United States, Canada, and far-eastern Russia. It is the only tick-borne virus to be endemic in North America. The cases occur primarily in the late spring, early summer, and mid-fall when ticks are most active due to the warmer weather. The seasonal incidence depends on the activity of tick vectors. Highest incidence is reported in rural or forested areas from June to September. There have only been 21 cases of Powassan disease in Canada since 2017 which means that the risk of the disease is very low in Canada. Males and children are more frequently infected possible because they tend to be more outdoors and up to 27 cases have been reported in North America since 1958.
Incubation Period
Powassan virus incubation period ranges from 1 – 4 weeks.
Reservoir and Transmission
The Blacklegged tick or deer tick is often responsible for biting and transmitting the disease to people. It primarily feeds on the white-footed mouse and the white-tail deer making them the most common reservoirs that infect the Blacklegged or deer tick with Powassan Virus. Other tick known to spread the disease are groundhog and squirrel tick which rarely bite humans. Ticks can attach to any part of the body but are often found in areas that are hard to see such as the groin, armpits, and scalp. Traditional ranges of ticks are expanding, and the incidence of Powassan disease is growing. This disease cannot spread from person to person as humans are considered “dead-end” hosts. However, Powassan disease can be transmitted through blood transfusions. Thus, people with confirmed Powassan virus infections should not donate blood for 6 months after their illness.
Laboratory Diagnosis
Laboratory tests detect antibodies in the blood or in the cerebrospinal fluid that the immune system makes against Powassan virus. According to CDC, the cerebrospinal fluid (CSF) or serum is tested to detect Powassan virus-specific IgM. Initial serological testing is performed using IgM capture enzyme-linked immunosorbent assay. A positive Powassan virus IgM antibody test result should be confirmed by neutralizing antibody testing of CSF specimens.
Molecular tests to detect viral RNA can be performed on serum, CSF, and tissue specimens that are collected early on in the illness. If positive, it confirms the Powassan Virus infection.
Prevention and Control
Prevention of Powassan Virus heavily depends on personal protective measures to decrease exposure to infected ticks.
- Reducing tick habitats near your home by keeping your lawn and yard well maintained to ensure the area is tick free.
- Protect yourself against tick bites which can be done by wearing light coloured clothing which makes it easier to spot ticks, going out more covered (long sleeved shirt and long pants with closed-toe shoes), and use an insect repellent containing DEET or Icaridin.
- Knowing what to do when bitten by a tick can also prevent the Powassan Virus infection. You should quickly remove the tick attached to your skin with clean tweezers, disinfect the site with alcohol or hand sanitizer, save the tick and record the date of the bite.
Vaccination
There is no vaccine to prevent the Powassan disease. Prevention of tick bites is the best prevention.
Treatment
There is no specific medication to treat Powassan Virus Disease. Treatment is not needed for people who do not develop symptoms. People with more severe symptoms will just have to be hospitalized to receive intravenous fluids (to stay hydrated), respiratory support (breathing support), and medications to reduce swelling in the brain.
- PHAC – Powassan Virus Treatment
- CDC – Powassan Virus Treatment
- CDC – Powassan Virus Treatment and Prevention
What is happening with current outbreak of Powassan Virus disease?
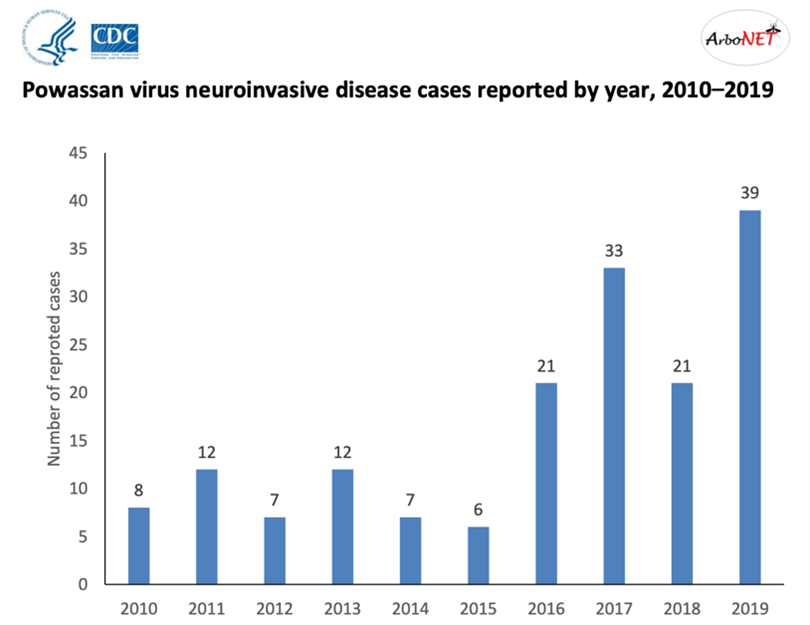
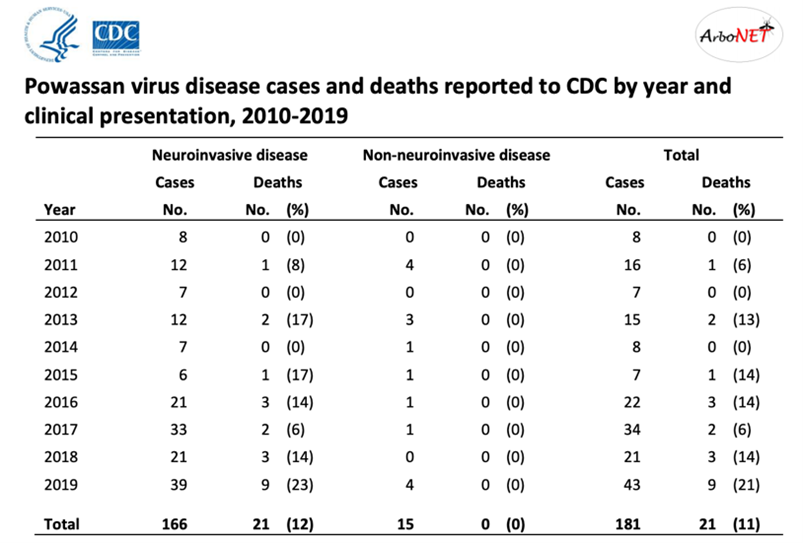
Powassan Virus Disease cases are rare, but the cases have increased in recent years. In the United States, the incidence of Powassan virus infections expanded from the estimated 1 case per year prior to 2005 to 10 cases per year during the subsequent decade. In Canada, specifically in southern Quebec, a 68-year-old woman was diagnosed with Powassan encephalitis in 2018.
- Quebec – Case of Powassan Encephalitis
- Tick-Borne Flaviviruses, with a Focus on Powassan Virus
- CDC – Statistics
- CDC – Reported Powassan Virus cases by state of residence
What is the current risk for Canadians from Powassan Virus Disease?
There have only been 21 cases of Powassan Virus disease in Canada since 2017 which means that the risk of the disease is very low in Canada. The risk of getting a tick bite starts in spring lasts through the fall (warmer weather).
Canadians who live, work or play outdoors in areas that are prone to ticks that spread the disease are at an increased risk for infection. However, the risk of acquiring Powassan disease is still much lower than Lyme disease which is another disease that infects humans via the bite of a blacklegged or deer tick. So this tick is known to spread both Powassan and Lyme disease however, the tick must be attached for 36 to 48 hours or more before the Lyme disease bacterium can be transmitted. Canadians need to be careful and take proper precautions when doing outdoor activities such as hiking, fishing, camping, hunting, gardening etc.
Squirrel and Groundhog ticks, which rarely bite people, are found in Ontario, Quebec, and Atlantic provinces.
Blacklegged ticks, which often bite people, are found in the southern parts of Quebec, Manitoba, British Columbia, and New Brunswick. It is also found in parts of Nova Scotia and southern, eastern, and northwestern Ontario.
Travel Restrictions
If traveling to the United States, be aware of the northeastern states and Great Lakes region as cases of Powassan Virus have primarily been reported from there.
What measures should be taken for a suspected Powassan disease case or contact?
Case and Contact Management
PHAC and CDC have developed brief guidelines to help healthcare providers in the management of the person infected with Powassan Virus. This includes diagnosis and reporting, clinical signs and symptoms, control, prevention, testing vaccination and reporting.
Powassan virus cannot spread from person to person as humans are considered “dead-end” hosts. It can only be transmitted via a bite of an infected tick. However, Powassan virus can be transmitted through blood transfusions. Therefore, people with confirmed Powassan virus infections should not donate blood for 6 months after their illness.
- PHAC – Powassan Virus Spread
- CDC – Powassan Virus Clinical Evaluation and Disease
- CDC – Powassan Virus Diagnostic Testing
- CDC – Powassan Virus Treatment and Prevention
Identifying and Reporting
Any person with fever-like symptoms or acute neurologic illness who potentially had likely exposure to ticks (primarily squirrel, groundhog, and blackhead tick) in Powassan virus endemic areas such as upper Midwest of United States, far-eastern Russia, and North America should be considered for Powassan disease.
Powassan virus disease is a nationally notifiable condition and therefore all Powassan Virus cases should be reported to local public health authorities in a timely manner.
Infection Control and Prevention
There is no vaccination or medication to treat Powassan Virus, so prevention and control of Powassan Virus heavily depends on personal protective measures to decrease exposure to infected ticks like avoiding wooded and bushy areas with high grass in endemic areas. Prevention of tick bites is the best precaution.
Powassan virus can be transmitted through blood transfusions. People with confirmed Powassan virus infections should not donate blood for 6 months after their illness.
